Guide to Current Procedural Terminology Codes for Speech Therapy
Comprehensive Guide to Current Procedural Terminology Codes for Speech Therapy
Navigating the complexities of medical billing and coding can be daunting for many speech-language pathologists (SLPs). Yet, it is crucial to ensure proper reimbursement for services rendered. Understanding the intricacies of medical billing helps SLPs receive fair compensation and leads to better patient care and healthcare outcomes.
Whether you're a seasoned professional or new to the field, mastering the fundamentals of billing can significantly impact your ability to secure the financial aspects of your practice. In this post, we will explore the basics of medical billing and coding for speech therapy services while highlighting key concepts and tips to empower SLPs to effectively manage this essential aspect of their practice.
Introduction to Medical and Billing Codes for Speech Therapy
Medical coding and billing are different but related processes. They both involve reporting diagnoses, procedures, and supplies to health insurance plans.
Medical coding is the process of reviewing a medical chart to extract billable information that can be translated into standardized billing codes.
Medical billing is the process by which providers of healthcare services submit claims to insurance companies to request reimbursement for services rendered. When the claims are submitted, billing codes are supplied to the payers.
Procedure codes inform the payer what service the healthcare provider performed, and diagnosis codes tell the payer why the patient received the services.
The main objective is for the provider or healthcare organization to receive all allowable reimbursement for the medical care given.
To be efficient, medical billers must first collect necessary information, including patient demographics, medical history, insurance coverage, and a list of the services or procedures the patient received.
Healthcare billing codes are a universal language among providers, billers, and payers (health insurance plans and self-pay clients). They standardize the description of procedures, diagnoses, and supplies.
Medical coding is the process of assigning a combination of alphanumeric values to a medical service. The Health Insurance Portability and Accountability Act (HIPAA) requires two main types.
The Healthcare Common Procedure Coding System (HCPCS) includes two levels:
Level I = Current Procedural Terminology (CPT) codes: used to identify the most common medical procedures
Level II = Codes used to identify equipment, supplies (Durable Medical Equipment or Orthotics), and some procedures not listed under CPT codes
CPT codes (HCPCS Level I)
Are published and updated by the American Medical Association (AMA)
Are usually five-digits
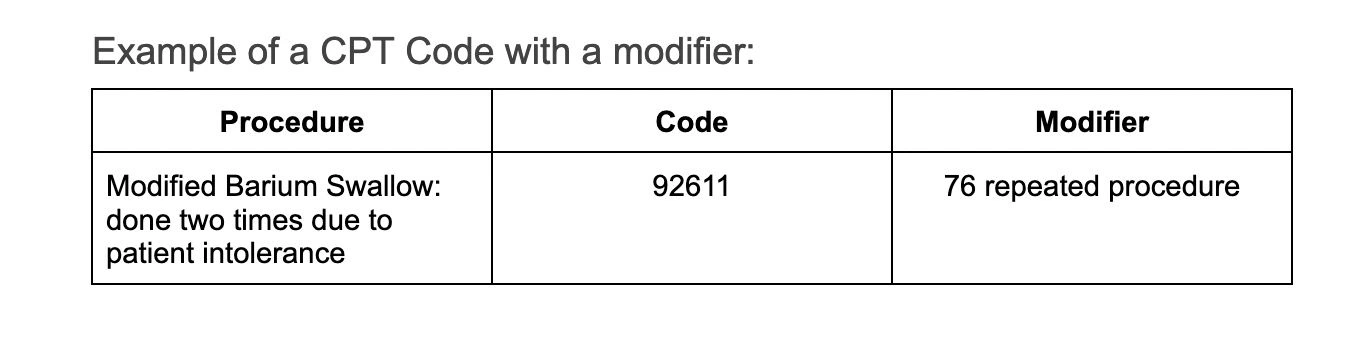
It may have 2-digit modifiers that indicate an unusual circumstance
Valued for reimbursement by the federal Medicare program
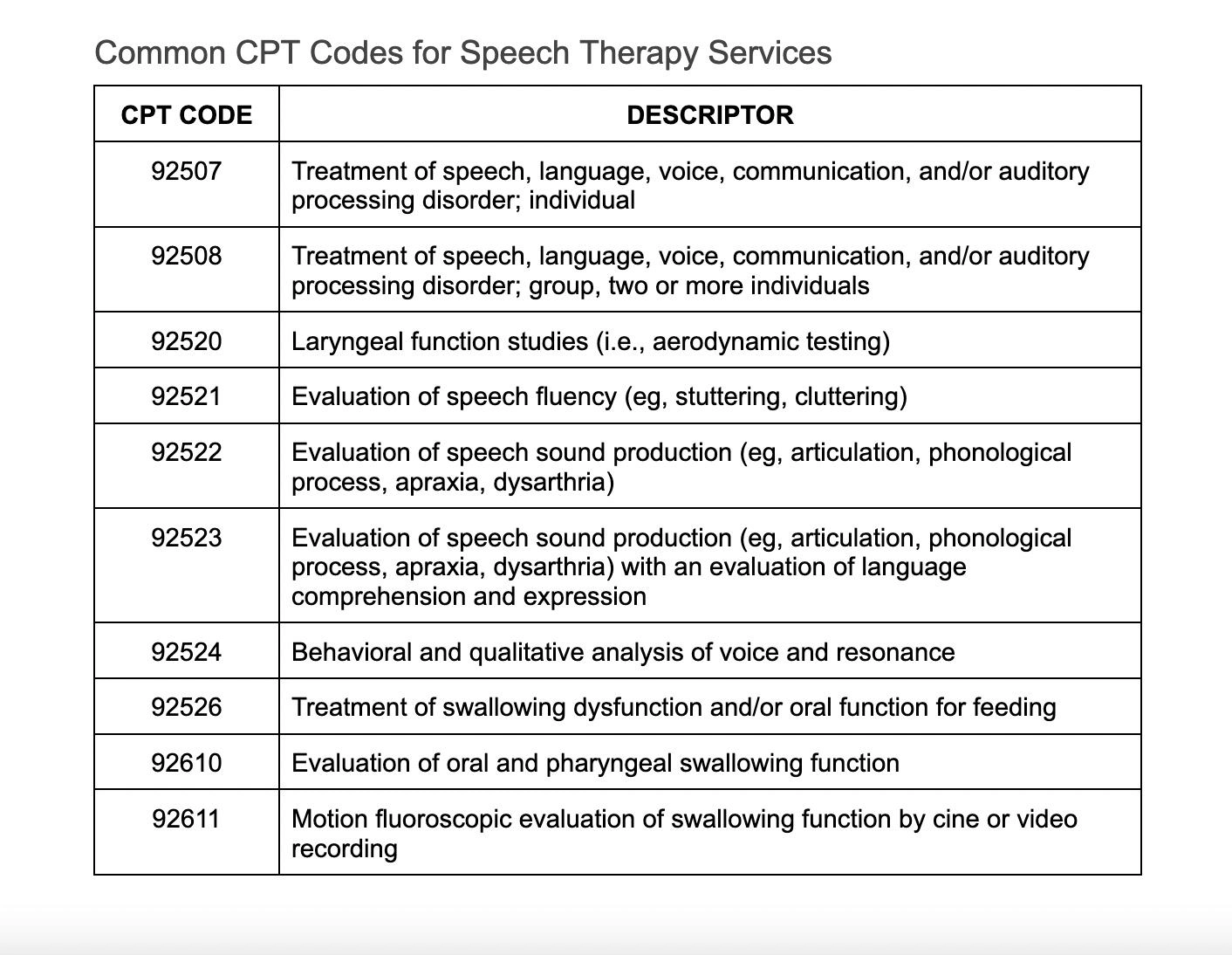
Choosing the correct CPT Code to Bill for Speech Therapy Services
After providing the service, select the descriptor that matches the procedure you just did.
If you cannot find a code to match your procedure (for example, Head Shake Test), you can use code 92700 for an unspecified otolaryngology procedure.
One procedure (evaluation, treatment, study) = one code
Some codes are time-based, while others are session-based. You must consider which is appropriate when performing the service and submitting your claim for reimbursement.
Speech Therapy CPT Code 2024 Update
New as of 2024: SLPs can provide and report caregiver training services for a single patient without the patient present. It must be provided under an established, individualized, and patient-centered plan of care. Speech therapists can provide caregiver training to an individual or a group of caregivers.
These new codes do not include a separate billing for discussions or brief education with caregivers immediately following a session with the patient. Instead, that would be included in the payment for the evaluation or treatment time with the patient.
SLPs will use the code for group caregiver training when conducting group training for the caregivers of multiple patients. The code would be billed once per patient represented, no matter the number of caregivers attended per patient.
These codes cannot be used to train medical professionals or caregivers who are employed to provide healthcare services to patients. The Center for Medicare Services (CMS) defines a caregiver as “a family member, friend, or neighbor who provides unpaid assistance to a person with a chronic illness or disabling condition.”
CMS requires that patients or their legal representatives provide documented consent for the caregiver to receive training without the patient's presence.
CPT Code Modifiers for Speech Therapy
Speech therapy modifiers are used when an HCPCS code needs to be supplemented to explain unusual circumstances that may apply to a service. Effectively using modifiers in speech therapy billing is essential because it guarantees precise and comprehensive details for payers. This results in proper reimbursement and acknowledgement of the medical necessity of the services rendered.
Some common modifiers used for speech therapy include:
GN - Service delivered personally by a speech-language pathologist or under an outpatient speech-language pathology care plan.
KX - The provider deems continued care medically necessary even though the financial threshold for therapy services has been met.
People with Medicare insurance have a threshold for therapy services. Once claims exceed that threshold, Medicare will not reimburse for additional services. In 2021, the combined cap for physical and speech therapy services was about $2000.
If a patient exceeds this cap, you would add the KX modifier to indicate that continued treatment is medically necessary. Your documentation must sufficiently justify that necessity.
GA - This modifier is used once the patient has reached a functional plateau but still wishes to continue with speech therapy services. It would not be used to bill Medicare. Instead, it can bill a secondary insurance or the patient directly.
22 - Increased Procedural Services. This modifier indicates a service that requires significantly greater effort, intensity, time, difficulty of procedure, severity of patient's condition, and physical and mental effort than is usually needed for that procedure.
95 - Telehealth services are provided in an outpatient, non-facility setting. This modifier will be used for a synchronous telemedicine service provided via a real-time interactive audio and video telecommunications system.
76 - Repeat the procedure by the same provider. This modifier means that the procedure was performed more than once by the same provider per date of service.
Medicare and Medical Billing for Speech Therapy
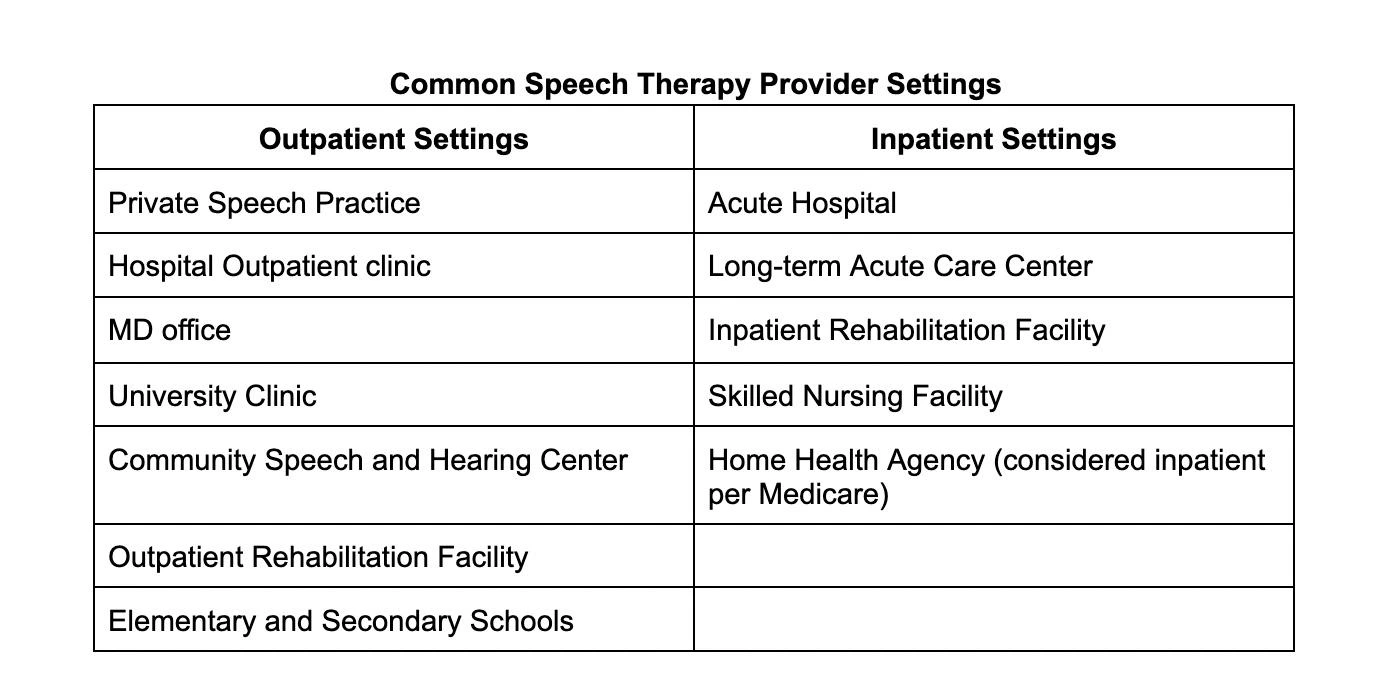
Medicare is a federal insurance for seniors over 65 and people with severe disabilities. The Medicare program heavily influences healthcare reimbursement. Medicare sets the example for what is covered and typical reimbursement rates. Commercial insurers and Medicaid often copy Medicare policies but can deviate from them based on their members’ unique needs.
Under the Medicare Program, an independent speech pathologist may bill Medicare directly. Additionally, speech-language pathologists' services may be billed by providers such as rehabilitation agencies, home health agencies, hospices, outpatient departments of hospitals, and suppliers such as physicians, and physical and occupational therapists in private practice.
The Medicare Physician Fee Schedule provides a list of rates for outpatient speech-language pathology covered under Medicare Part B. It is categorized by the relative CPT codes that a provider may bill. SLPs can use this as a guide to help establish their outpatient service fees.
Additionally, there are a few other potential payers to be aware of:
SLP services are covered by Medicare Part A when the patient is in an inpatient setting.
Medicaid is the federal and state program that pays for the healthcare of impoverished people. Speech therapy is considered an optional Medicaid benefit. Each state determines whether it will cover the service and the criteria under which it is covered.
Private (Commercial) health insurance plans such as United Healthcare or Humana also have the option to choose whether to cover speech therapy and may require prior authorization before approving services.
In some cases, the patient pays for the services directly.
ICD-10-CM: Diagnosis Codes
International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM): The World Health Organization assigns diagnostic alphanumeric codes to diseases, injuries, and disorders. Diagnosis codes are used in conjunction with CPT codes to justify services provided.
Common ICD-10 Diagnosis codes treated by Speech Therapists
F80.1 Expressive Language Disorder
F80.2 Receptive Language Disorder
F80.4 Speech and Language Developmental Delay Due to Hearing Loss
R48.2 Apraxia
R13.1 Dysphagia
R47.1 Dysarthria
T17. 2 Foreign body in pharynx
General Rules of Thumb for selecting the correct ICD 10 CM code for billing:
Prioritize the diagnosis code based on the chief complaint or reason for the visit. If multiple problems exist, they may be listed as secondary diagnoses.
For example, you are treating a child with speech delay. The primary diagnosis may be expressive language disorder, ICD code F80.1; The secondary diagnosis: Autism, ICD code F84.0
Use the code with the highest degree of medical certainty. Based on your assessment of the patient, choose the most specific code possible.
F80: Specific developmental disorders of speech and language
F80.0: Specific speech articulation disorder
F80.1: Expressive language disorder
F80.2: Receptive language disorder
F80.3: Acquired aphasia with epilepsy
Avoid using nonspecific codes when possible (not otherwise specified-NOS or not elsewhere classified-NES). If you have enough information, choose a more specific code.
Example: R49.1 Aphonia (Loss of Voice) is a better choice than
R49.8 Other and unspecified voice disturbances (Change in voice NOS), if appropriate, based on the patient’s condition.
NOS (not otherwise specified) may be used when the medical provider does not adequately describe the condition, or the medical record's information is insufficient to assign a more specific code.
NES (not elsewhere specified) may be used when no appropriate code was found on the list. Based on the information provided in the medical record, there is no more specific code available.
Non-physician providers (such as Speech Language Pathologists) may use signs, symptoms, and undefined conditions as a chief complaint. (Medical providers only use medical conditions or injuries)
Example: You evaluate because of pain in the throat. Testing is done during the visit, and the results are normal. You would code the symptom, R07.0 Pain in Throat, as the chief complaint and discuss the normal clinical results in the clinical notes.
The diagnosis code should match the accompanying procedure code; otherwise, the claim may be denied. This seems obvious, but it is an easy mistake. For example, if a therapist is treating someone who is admitted to the hospital for breast cancer but referred to speech after an episode of choking. The chief complaint would be choking, not breast cancer.
Avoid being accused of submitting Fraudulent Claims:
Do not use diagnosis codes for conditions that were previously treated and no longer exist
Do not use diagnosis codes for conditions that are probable, suspected, or rule out diagnoses
Do not use CPT codes that misrepresent the service that was provided to receive reimbursement
Documentation that Supports Billing for Speech Therapy
Clear and concise documentation is necessary to verify your services for the payer.
Documentation aims to provide a comprehensive report that helps justify the services planned for the patient. Clinical reports and notes facilitate communication and continuity of care among providers. Adequate documentation summarizes critical and essential information so that it is easy for physicians, payers, and others to interpret. Be as succinct as possible while including all the necessary details of the evaluation or treatment.
Prepare for Utilization Review
The payer will analyze the patient's symptoms and the kinds of services provided to determine medical necessity. If the necessity of your services is challenged, the clinical notes will be provided to support your claim. If you are audited, your clinical notes must prove that you did what you billed for.
Documentation Required by Health Plans to Support Medical Necessity
Evaluation report: This report includes standardized tests and informal evaluations, the provider's interpretation of the findings, and the provider’s recommendations based on those findings.
Treatment Plan: the provider's plan of care to improve the condition should include the diagnosis, short-term and long-term goals, the services type, amount, duration, and frequency
Progress Notes: Each time the patient is seen, notes should be taken about activities that take place during the session and the patient's current functional status. In some settings, you must include a start and end time.
Progress Notes should include:
State the reason for the encounter (the condition being evaluated)
Document the services correctly to be able to derive CPT and ICD codes
Provide a basis for medical necessity
Discuss the plan of care
Discharge Summary: summarizes the services provided, progress made toward goals, and current functional status
Best practices for clinical documentation:
Completed at the time of service
Includes all historical events, including phone conversations with patients or other providers
All entries are dated and signed
Reflect the complexity of services and time spent,
Physician’s Orders
In general, SLPs are not required to have a physician’s order to provide services. However, a third-party payer or facility providing care may require it. When required, the MD order needs to provide the SLP-related diagnosis.
Medical billing documentation requirements vary by setting, but they are usually driven by the payer in that setting.
The Superbill
The facility billing department usually manages coding for inpatient services. However, private Speech Therapy providers may have office staff to assist with submitting claims. Many providers use a Superbill, a document that lists the services and fees for the most common CPT codes billed by the office, to assist them with selecting and documenting the correct service code. It is a valuable tool for submitting claims and keeping track of the services provided.
CMS Form 1500
A non-institutional provider with less than ten full-time employees can use CMS Form 1500 to bill Medicare, Part B, for speech therapy services. The form can be obtained from the US Government Printing Office or online.
When documenting CPT codes, SLPs must be mindful of the amount and types of codes that can be billed on the same day. Some codes are time-based. For example, if a patient is seen for an evaluation of auditory function for surgically implanted device candidacy and the time spent was 1 hour and 30 minutes, the biller would submit a claim using:
Code 92626 for the first hour
Code 92627x2 for each additional 15 minutes
Same-Day Billing Requirements
Healthcare providers who submit claims health plans should be aware of restrictions related to services provided on the same day. When two services cannot reasonably be performed during the same encounter, they are mutually exclusive and will not be reimbursed if billed on the same date of service. The National Correct Coding Initiative (NCCI) system regulates the same-day billing requirements for Medicare and Medicaid services. Code pairs that cannot be billed by an individual provider in an outpatient setting on the same day for the same patient are called Corrective Coding Initiative Edits (CCI edits). They only apply to some CPT codes, but not all.
Meeting Criteria for Medical Necessity
For a payer to approve reimbursement, the documentation must show that the services provided meet medical necessity criteria. Here is a sample of criteria for Speech Therapy from the Center for Medicare (CMS) website.
Speech-language pathology services may be considered reasonable and necessary when the following criteria are met:
The services shall be considered under accepted standards of medical practice to be a specific and effective treatment for the patient's condition.
The services shall be of such a level of complexity and sophistication, or the patient's condition shall be such that the required services can be safely and effectively performed only by a qualified therapist.
Medicare coverage does not depend on the presence or absence of a beneficiary’s potential improvement from therapy but rather on the beneficiary’s need for skilled care. The amount, frequency, and duration of the services must be reasonable under accepted standards of practice.
In the case of rehabilitative therapy, the patient’s condition has the potential to improve or is improving in response to therapy; maximum improvement is yet to be attained, and there is an expectation that the anticipated improvement is attainable in a reasonable and generally predictable period of time; or The services must be necessary for the establishment of a safe and effective maintenance program required in connection with a specific disease state, including evaluation, plan of treatment, and staff and family training, when the skills of an SLP are required.
In the case of progressive degenerative disease, service may be intermittently necessary to determine the need for assistive equipment and/or establish a program to maximize function.
In the case of maintenance therapy, treatment by the therapist is necessary to maintain, prevent, or slow further deterioration of the patient’s functional status, and the services cannot be safely carried out by the beneficiary him or herself, a family member, another caregiver, or unskilled personnel.
Frequently Asked Questions When Billing for Speech Therapy Services:
Where can I find a list of current, frequently used CPT and ICD-10-CM codes related to speech therapy services?
The American Speech-Language-Hearing Association (ASHA) has a wealth of resources on its website to assist with billing and coding specifically for SLPs. Here are a couple of tools to help you get started:
Medicare CPT Coding Rules for Speech-Language Pathology Services
2023 ICD-10-CM Diagnosis Codes Related to Speech, Language, and Swallowing Disorders
How can I access the Medicare Physician Fee Schedule to determine the rate Medicare will pay for each CPT code billed?
ASHA provides a downloadable document with extensive information about the reimbursement rates and their determination.
2024 Medicare Fee Schedule for Speech-Language Pathologists
When providing caregiver training to a set of parents, do I bill 1 code per session or 2 codes (one for each parent)?
In this situation, you would bill 1 code per session for the patient's caregivers.
What are some common reasons that a Speech Therapy Claim gets denied?
There are a variety of reasons that a medical claim can be denied reimbursement, but here are some common reasons:
The payer does not cover speech therapy services
The payer requires prior authorization, but it was not requested
The payer disagrees that speech therapy is medically necessary to treat the patient’s condition
The claim has incorrect or missing information
The provider has billed for a time-based code when a session-based code is more appropriate
The provider has billed for more services than are supported by the documentation provided
The patient is not making progress or showing significant improvement over a set period of time
The service being provided can be carried out by the caregiver
Can a speech-language pathologist hire a speech-language pathology assistant and be reimbursed, and what are the regulations?
Medicare does not reimburse for services provided by speech-language pathology assistants. They are not considered medically necessary and, therefore, are not reimbursable. You must check with the payer for private healthcare plans to determine their provider requirements. Usually, private healthcare plans will make determinations similar to Medicare’s regarding provider requirements.
If the payer denies my claim for reimbursement, what can I do?
When you receive a denied claim, review the medical record to determine whether there was an error. If so, correct the billing error and resubmit the claim, ideally within one week of the denial.
If you cannot determine the cause, contact the payer to request additional information about the reason for denial and the appeals process, if needed.
Sources
American Speech-Language-Hearing Association
The right time for billing codes
Like this project
Posted Jul 9, 2024
Monique researched the most current regulations on medical billing for speech therapists and created this comprehensive guide for a client.
Likes
0
Views
20