Usefulness of virtual autopsy in diagnosing pathologies in the …
Chathula Ushari Wickramasinghe
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
1,✉, Deepthi Edussuriya
Deepthi Edussuriya
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
1, Sriyani Perera 2, Nimashi Herath
Nimashi Herath
1Department of Forensic Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
1
Abstract
Objective:
Virtual autopsy is a non-invasive/minimally invasive method for conducting an autopsy, with the assistance of imaging techniques. We aim to review the benefits of virtual autopsy in detecting pathologies in the paediatric population.
Method:
The procedure adhered to Institute of Medicine and Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines. Seven databases including MEDLINE and SCOPUS were searched for articles published 2010–2020 worldwide in English. A narrative synthesis of the findings of included studies was carried out to discuss and summarize the results of the review.
Results:
From 686 studies on paediatric deaths, 23 met selection/quality criteria. Virtual autopsy was better than conventional autopsy in detecting skeletal lesions and bullet trajectory, thus a crucial tool in the investigation of traumatic and firearm deaths. Virtual autopsy was superior to conventional autopsy in identifying the point of bleeding in postoperative deaths and objectively quantifying air/fluid in body cavities. Virtual autopsy was a useful adjunct for detecting pulmonary thrombo-embolism, foreign body aspiration, drowning and metastatic malignancies. The use of non-contrast imaging in investigating natural paediatric deaths did not offer more information than conventional autopsy. Misinterpretation of normal post-mortem changes as pathological findings was another disadvantage of virtual autopsy leading to erroneous conclusions. But accuracy may be improved with contrast enhancement and post-mortem magnetic resonance imaging.
Conclusion:
Virtual autopsy is a crucial tool in the investigation of traumatic and firearm deaths in the paediatric population. Virtual autopsy will be useful as an adjunct to conventional autopsy in asphyxial deaths, stillbirths and decomposed bodies. Virtual autopsy has limited value in differentiating antemortem and post-mortem changes with the added risk of misinterpretations, therefore should be used with caution in natural deaths.
Keywords: Virtual autopsy, conventional autopsy, paediatric, imaging
Introduction
Since the 1300s autopsies, also known as necropsies, have been carried out as part of death investigations for both academic and medico-legal purposes. 1 In the last three decades, the development of technology has made a significant impact on the evolution of autopsy techniques. Richard Dirnhofer first introduced the concept of ‘virtual autopsy (VA)’ or ‘virtopsy’ by combining innovative technology with conventional autopsy (CA). The result is a non-invasive method of conducting autopsies employing imaging modalities such as X-ray, computed tomography, magnetic resonance imaging and so on. 1
VA has many uses, as an adjunct to CA to accentuate the findings of CA and enable targeted system-specific CA. Although for medico-legal autopsies the consent of the family is irrelevant, pathological autopsies, conducted to gain a better understanding of the disease process, require the consent of the family to proceed. When cultural, religious and other factors prevent or limit the conduct of CA in pathological post-mortems (PMs), VA can act as a substitute. 2 The early stage of the prevailing COVID-19 pandemic illustrates such an instance where VA substituted CA in some cases, as the risk of infection restricted the conduct of full CA. 3 According to the literature, the extent and the reason for the use of VA in different countries vary significantly. Being increasingly used in developed countries due to the high availability and accessibility of imaging modalities, VA is useful either as an alternative or as an adjunct to CA. In contrast, Japan, which has a very low PM rate compared to Western countries and widely available imaging equipment, uses VA either as an alternative to CA or to screen for the need for a CA. 4 Therefore, it is evident that based on various factors such as the availability of technology, expertise and PM rate, the use of VA should be customized to each country to obtain the maximum benefits.
However, there is a vast difference between the application of VA in adult and paediatric populations. This is due to the differences in disease pathologies between the two populations. The wide spectrum of causes responsible for paediatric mortality including congenital structural anomalies, syndromic pathologies and so on necessitates the use of radiological techniques for a full and complete death investigation. Although there is a strong need to determine the cause of paediatric deaths, there is a general reluctance among parents and family to proceed with a full traditional autopsy, thus making less invasive VA a better option in such instances. 5
The cost of equipment, technology, infrastructure and training/expertise are the main drawbacks of VA, especially for developing countries, making such imaging modalities less available and accessible to forensic pathologists. Furthermore, the inability to perform sampling for histopathological studies and the inability to appreciate physiological characteristics such as smell, texture and colour are some other disadvantages. Also, in some instances, the distinction between antemortem (AM) and PM changes is not detected in VA leading to misinterpretations. 6
Therefore, it is important to obtain a thorough understanding of the uses of VA to ensure the judicious use of valuable resources while ensuring accuracy in diagnosis. We aim to review the benefits of VA in detecting pathologies in the paediatric population.
Methods
All four authors (DE, CW, SP and NH) contributed to creating the review protocol according to Preferred Reporting Items for Systematic Review and Meta-Analysis protocols (PRISMA-P 2015) statement. 7 It was registered in the PROSPERO registry (CRD42021236545),
The methodology followed the guidelines and standards of the 1175778 Institute of Medicine 8 and PRISMA-2015 was used for reporting.
Search strategy
The aim was to identify studies examining the usefulness of VA in diagnosing pathologies in paediatric deaths. The key search terms were identified with the aid of a search-term-harvesting table by DE and CW. A systematic and comprehensive search was conducted by SP and VA, and references were managed using the reference management software Mendeley. The following databases were searched.
Cochrane Database of Systematic Reviews, The Database of Abstracts of Reviews of Effects, MEDLINE (1950–2020) via PubMed (see Supplemental Appendix 1 for search strategy), The Cochrane Central Register of Controlled Trials (1948–2020), Scopus, LILAC and Index Medicus for Southeast Asian region. The search was conducted on 1 June 2020, with no beginning date limit imposed. The search terms used were ‘Virtual autopsy (or VA)’ or ‘Virtopsy’ or ‘post-mortem imaging’ or ‘computed tomography’ (or CT) or ‘computerized tomography’ and ‘post-mortem computed tomography’ (or PMCT). A combination of relevant medical subject headings and search terms tagged with other appropriate search fields was used in the literature search (see Supplemental Appendix 1 for search strategy). Additionally, the reference list of each selected article was checked manually for other relevant publications (cross-reference search) to identify additional studies that may have been missed in the computerized database search.
Selection criteria
After the removal of duplicates from the retrieved articles, the remaining articles with abstracts were uploaded to the web application, Rayyan 9 for screening. The criteria for the selection of articles were based on the PICOST elements: Participants – medico-legal autopsies, paediatric population, Intervention – VA, Comparison – CA and Outcome – usefulness in medico-legal practice, Setting – worldwide, Time – 2010–2020. Studies that assessed the usefulness of VA in diagnosing pathologies in the paediatric population were selected for inclusion if the full text was available. Only articles published in English and human cadavers aged 0–18 years, both male and female were included. Unpublished data were excluded from this review.
DE and CW independently screened the uploaded articles in Rayyan, using the above eligibility criteria. In the first phase, the title and abstract of each article were reviewed by the two authors independently for their candidacy. The full texts of all those selected articles were retrieved by CW and further examined by the same authors independently (second phase), for the final verification before inclusion in the review. Any disagreements regarding the decision on the eligibility of studies were resolved by consensus. Reviews, systematic reviews, editorials, letters, and comments were removed. Only the articles which met the eligibility criteria were selected for inclusion in the review. Excluded studies were marked with the ‘reason’ in Rayyan.
Data extraction and quality assessment
Data from all included studies were extracted by the two review authors CW and NH using a data extraction table developed for this review. Data extracted were cross-checked by the same authors for any errors. The information recorded included: Study details (author, year, country of origin), Methods (study aim, study design, the imaging technique used to determine the autopsy and the presence or absence of traditional autopsy, including the comparison), Study type: Intervention studied, Outcomes: all relevant findings related to usefulness in diagnosing paediatric pathologies (as primary or secondary outcomes).
Quality assessment (QA) Checklists of the Joanna Briggs Institute Critical Appraisal tools for use in systematic reviews 10 were applied to assess the quality of the selected studies. CW and DE independently assessed the quality of each of the selected studies, the results of the QAs were recorded and compared, and in case of a disagreement, a third reviewer SP was consulted. For QA, the overall description of the study methods, results and discussion were analysed. Based on the results of the QA process, only the studies which met the quality criteria were selected for inclusion in the review. Studies that were considered of poor quality were excluded.
Strategy for data synthesis
Due to the heterogeneity between the included studies, quantitative synthesis was not considered. A narrative synthesis of the findings from individual included studies was carried out by DE and CW. Data were analysed under two main circumstances, natural deaths and unnatural deaths. The usefulness of VA was categorized as ‘useful’, ‘equivalent’ and ‘not useful’.
Results
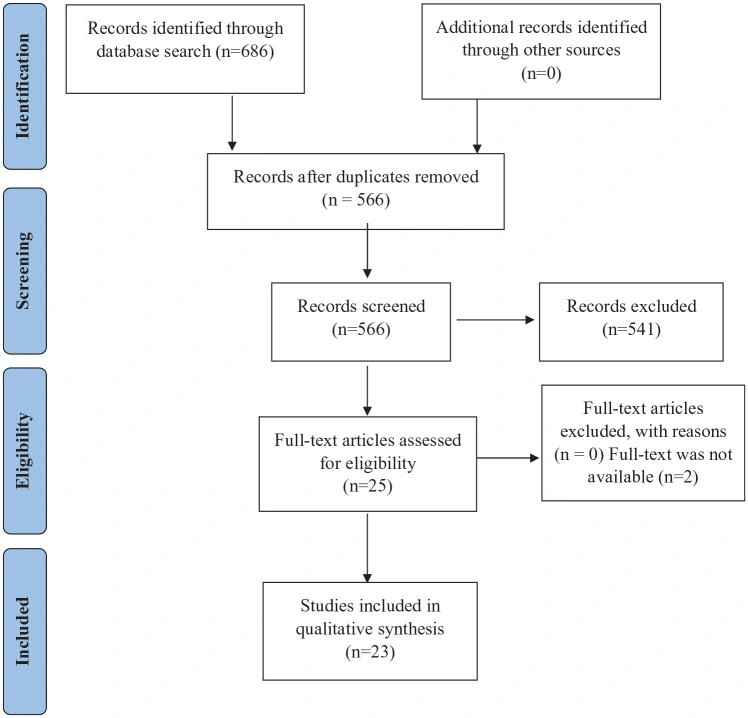
The literature search resulted in a total of 686 articles. After removing the duplicates, 566 articles were considered for screening using the eligibility criteria. The initial evaluation of articles through title and abstract resulted in only 25 articles meeting the selection criteria. After full-text evaluation 23 studies were selected. The QA confirmed the candidacy of all 23 studies for inclusion in the review. The flow diagram of the selection of studies is shown in Figure 1.
The characteristics of the included articles are demonstrated in Table 1. The articles included in the review were from developed countries with the majority being from Europe (n = 18) and the rest from the United States (n = 4) and Asia (n = 1). The study types included mainly cross-sectional (CS) analytical (n = 9), CS descriptive (n = 6) and case reports (n = 8). The imaging techniques used for the conduct of VA included PM magnetic resonance imaging (PM-MRI) (n = 10), PMCT (n = 10), a combination of PMCT and X-ray (n = 1) and a combination of PMCT and PM-MRI (n = 2).
Table 1.
Characteristics of the included studies.
Source (author) Country Study design Sample size VA technique used Was CA done Mean age/age range Post-mortem Interval Rutty et al. 11 United Kingdom Case report 1 PM-MSCT Yes Newborn <10 h Ebert et al. 12 Switzerland Case report 1 PMCT
PM-MRI Yes 13 years – Nascimento et al. 13 United States Case report 1 PMCTA Yes 18 years – Filograna et al. 14 Italy Case report 1 PMCT No 18 months 12 h Davis et al. 15 United States Case report 1 PM-MRI No 1 day 24 h Andronikou et al. 16 United Kingdom + South Africa Case report 1 PM-MRI No 10 years 12 h Harty et al. 17 United States Case report 1 PMCT Yes 15 years 4 h Del Fante et al. 18 Italy Case report 1 PMCT Yes 17 years – Sieswerda-Hoogendoorn et al. 19 Netherlands CS descriptive 12 PMCT Yes Newborns (mean – 38 weeks of gestation) 3 weeks–7 years (estimated) Montaldo et al. 20 United Kingdom CS analytical 14 PM-MRI Yes 3 days (1–4 days) 3 days Tumanova et al. 21 Russia CS analytical 18 PM-MRI Yes 1–54 days 6–15 h Tumanova et al. 22 Russia CS analytical 23 PM-MRI Yes 6 h 45 min to 36 days 6–15 h Krentz et al. 23 Brazil + Switzerland CS analytical 26 PMCT Yes 34.8 months <3 days Arthurs et al. 24 United Kingdom CS analytical 29 PMCT
PM-MRI Yes 6.9 months – Leadbetter et al. 25 United States CS descriptive 31 PM-MRI Yes 9 days
(0.13–180 days) 10 ± 6.6 h Simanovsky et al. 26 Israel CS analytical 35 PMCT No <3 years – Proisy et al. 27 France CS descriptive 47 PMCT
X-ray Yes 6.2 ± 5.9 months 24–72 h Rjin et al. 28 Netherlands CS descriptive 54 PMCT Yes 1.1 years (boys)
0.8 year (girls) – Sieswerda-Hoogendoorn et al. 29 Netherlands CS analytical 98 PMCT Yes 1 year 1 month (3 months to 6 years) 0–7 days Thayyil 30 United Kingdom CS analytical 123 PM-MRI Yes <1 month (34%), 1–12 months (43%), 12 months to 16 years (23%) 4.5 days Taylor et al. 31 United Kingdom CS analytical 123 PM-MRI Yes Arthurs et al. 32 United Kingdom CS descriptive 123 PM-MRI Yes Arthurs et al. 33 United Kingdom CS descriptive 123 PM-MRI Yes
MSCT: multi-slice computed tomography; PMCTA: post-mortem computed tomography angiography.
The articles discuss the investigation of unnatural and natural deaths, two postoperative deaths as well as 36 cases where the cause of death (COD) was unascertained. Deaths following road traffic accidents (RTAs), firearm injuries, child abuse, asphyxia and stab injuries have been discussed under unnatural deaths. The majority of natural deaths involved congenital abnormalities, followed by infections and bowel pathologies (Table 2).
Table 2.
Case distribution according to the manner of death.
Type of death Cause of death Sample size Unnatural deaths RTA 02 Foreign body aspiration 01 Sport-related 01 Firearm 03 Drowning 01 Asphyxia 02 Stab 02 Chest wall trauma 01 Manual strangulation 01 Neonaticide 12 Child abuse 46 Child abuse/trauma 24 Natural deaths Pulmonary embolism 01 ● Congenital abnormalities
● Brain and spinal cord
● Cardiac
● Pulmonary
● Abdominal wall defect
● Renal malformations
● Musculoskeletal
● Anasarca
● Diaphragmatic hernia with lung hypoplasia
● Non specified
29
10
06
02
06
03
18
17
06 Infections 56 Metastatic disease 02 Bowel volvulus 02 Intestinal atresia 02 Intestinal malrotation 03 Acute abdomen 06 Liver necrosis 04 Adrenal haemorrhage 06 Pulmonary haemorrhage 12 Neonatal encephalopathy 07 Sudden unexpected neonatal death 07 Acute tubular necrosis 02 Other 517
From the 23 articles reviewed, 6 articles discussed the investigation of unnatural paediatric deaths, 12 articles discussed natural paediatric deaths and 5 articles discussed both natural and unnatural deaths. VA was recognized as a crucial tool and a useful adjunct, especially in the investigation of unnatural, traumatic deaths with skeletal lesions. However, in the investigation of natural paediatric deaths, it was observed that VA was helpful in arriving at a final COD, did not offer additional information compared to CA, and also in some instances led to misinterpretation of normal PM changes. Several articles discussing natural paediatric deaths identified VA as a useful tool for the detection of metastatic malignancies, when circumstances limit/prevent the conduct of CA, quantitative assessment of fluid/gas in body cavities, cardiac structural anomalies and detection of pathologies when in an advanced state of decomposition. The findings of the 23 reviewed articles are summarized in Table 3.
Table. 3.
Summary of findings of the included studies.
Ref. no. Sample size Mechanism of death Interventions Summary of findings 18 1 Firearm PMCT + PM • PMCT with image reconstruction was able to accurately demonstrate the bullet entry point, exit point and trajectory.
• This enabled more reliable event reconstruction.
• Facilitated more objective and reliable detection and quantification of pneumothorax.
• Was able to better demonstrate parenchymal and skeletal injuries. 27 14 Natural PMCT + X-ray • PM changes similar to those observed in adults were noted including hyper-attenuation of the aortic wall, hypostasis and clotting in the heart and vessels.
• Was able to detect skeletal lesions associated with death following NAI.
• Highest discrepancy between PMCT and CA findings was observed in cases of pneumonia.
• Interpretation of lung pathologies (non-traumatic) was found to be challenging due to the presence of PM changes.
• Poor resolution of cardiac pathologies with PMCT was observed.
• In the unascertained deaths, combined use of CA, VA and histology was unable to detect a reliable COD. 4 Child abuse 29 Unascertained 23 9 Traumatic
RTA – 2
Firearm – 2
Stab – 2
Sport-related – 1
Strangulation – 1
Post-op – 1 PMCT + PM • Better than CA in detecting skeletal lesions.
• Limited detection of organ parenchymal pathologies and cardiac pathologies.
• Difficulty in differentiating AM and PM lesions.
• Misinterpretation of normal PM findings.
• Less value in asphyxia, natural deaths (mainly cardiac), acute bronchopneumonia, and aspiration. 14 Natural 2 Asphyxia 1 Unascertained 13 1 Post-op PMCTA + PM • Useful in identifying the point of bleeding in post-op haemorrhage. 15 1 Natural (neonatal neuroblastoma) PM-MRI • Useful when circumstances limit/prevent CA.
• Allows limited sampling for histology.
• Able to detect the extent of metastatic disease. 16 1 Natural (chordoma) PM-MRI • In malignancies, useful in detecting the primary site and metastatic spread. 21 18 Natural (9 with anasarca, 9 without) PM-MRI + PM • Better than CA for quantitative assessment of anasarca 22 17 LH + DH PM-MRI + PM • Useful to diagnose lung hypoplasia associated with diaphragmatic hernia.
• Can be used to assess treatment efficiency of lung conditions in an innate diaphragmatic hernia. 6 Congenital ab/n 31 123 Natural PM-MRI • No major structural cardiac abnormalities were missed with VA.
• 8 cases of myocarditis (2%) were not detected with VA 30 108 Natural PM-MRI • Useful for detection of pathologies especially when autolytic changes affect the histological examination.
• Concordance between VA and CA findings was slightly lower in children compared to foetuses.
• Furthermore, this concordance was observed to decrease with increasing age.
• The reason was poor detection of sepsis affecting lung and/or heart, intestines or disseminated sepsis using VA. 15 Traumatic 33 123 Natural PM-MRI • PM-MRI was good at detecting renal pathologies.
• Poor at detection of intestinal pathologies.
• The overall sensitivity and specificity for abdominal pathologies was, respectively, 72.5% and 80%. 24 29 Natural PMCT
PM-MRI • Diagnostic accuracy of PM-MRI was higher than that of PMCT.
• Higher number of PMCT examinations (than PM-MRI) were non-diagnostic. 12 1 Traumatic PMCT
PM-MRI • Cardiac laceration following blunt force trauma to the chest was detected by both VA and CA independently.
• The amount of hemopericardium was measured using VA. 14 1 Drowning PMCT • VA detected frothy fluid in airways and ground glass opacities in non-dependent areas of the lungs and haemodilution.
• VA was useful in excluding other forensically significant lesions/injuries. 11 1 FB aspiration MSCT + PM • MSCT was able to detect the presence and location of FB in the upper airway of the newborn.
• VA failed to detect the type and number of foreign bodies present.
• VA was able to accurately detect PIE which can be helpful in differentiating whether it was a live birth. 29 51 Unnatural
Child abuse – 42
Accident/abuse – 9 PMCT • Useful in traumatic deaths, with a high level of agreement with CA findings in unnatural deaths.
• Diagnostic accuracy of VA in natural deaths is low.
• 37% false negatives in unnatural deaths.
• Where no COD was detected with CA, VA failed to identify any positive findings in 98% of cases. 35 Unascertained 12 Natural 19 12 Neonaticide PMCT • Useful for the estimation of gestational age in states of advanced decomposition.
• Useful to differentiate between still and live birth in states of advanced decomposition. 26 35 Natural (unspecified) PMCT • Tapering of the aortic arch which is considered as a normal PM change can be misinterpreted as hypoplastic aortic arch. 20 7 NE PM-MRI + PM Cannot differentiate AM hypoxic brain injury from PM changes. 7 SUND 28 54 Natural (unspecified) PMCT + PM • In 12% of cases COD was identified using PMCT.
• In another 12% of cases PMCT was able to detect positive findings but they did not have any contribution to the COD.
• In 74% of cases PMCT was unable to add to the final COD. 17 1 Natural – PE PMCT + PM • PE was detected with VA only during the second reading by a more experienced forensic radiologist.
• This highlights the importance of specialized training for a positive outcome.
• Normal PM changes seen in PMCT chest including dependent layering of blood in the left atrium, hyper-attenuation of the aortic wall and left ventricular hypertrophy may be misinterpreted by a less experienced person. 25 31 Natural (unspecified) PM-MRI + PM • Better at detecting pneumothorax, pneumoperitoneum and hepatic iron overload.
• Inferior to CA in detecting pulmonary vascular changes in PHT, focal bowel necrosis and perforation, focal pulmonary haemorrhage, pulmonary consolidation and hypoxic–ischemic injury.
• Family survey revealed that the majority of families preferred the combined use of VA and CA in the death investigation rather than either one alone. 32 123 Natural PM-MRI • Poor detection of common non-cardiac thoracic pathologies with VA with a sensitivity and specificity of 39.6% and 85.5%, respectively.
• Among non-cardiac thoracic pathologies, VA was most useful in detecting structural abnormalities, including pleural effusions and lung hypoplasia.
• VA was least useful in detecting infection.
MSCT: multi-slice computed tomography; PMCTA: post-mortem computed tomography angiography; PIE: pulmonary interstitial emphysema; PHT: pulmonary hypertension; PE: pulmonary embolism; SUND: sudden unexpected neonatal death; NE: neonatal encephalopathy; post-op: postoperative; NAI: non-accidental injury; LH: lung hypoplasia; DH: diaphragmatic hernia.
Discussion
In this review, we found that several studies have conducted both VA and CA to demonstrate the usefulness of VA in the investigation of unnatural deaths as well as natural deaths.
VA in unnatural deaths
In the PM investigation of a case of firearm-related fatality in a 17-year-old boy, PMCT with three-dimensional (3D) reconstruction has proved to be beneficial in determining the entry and exit points with a clear demonstration of the bullet trajectory. 18 This has enabled the accurate and objective reconstruction of the event. In addition, PMCT could better detect other firearm-associated injuries such as skeletal lesions and pneumothorax compared to CA. 18 Therefore, VA should be considered a mandatory tool in the investigation of such deaths involving complex event dynamics.
However, in some instances, the use of VA has failed to provide any additional information compared to CA. For example, the combined findings of PMCT and PM-MRI were able to report only the findings compatible with that of CA, and no additional information has been revealed. 12
The investigation of deaths following drowning is challenging for both CA and VA. In the one case of drowning death included in the review, it was observed that although PMCT would show the typical appearance of frothy fluids in airways and ground glass opacities in non-dependent areas of the lungs, CT imaging alone is not sufficient to differentiate the nature of the aspirated material with absolute confidence, as frothy fluids and semi-liquid gastric material can give a similar appearance. 14 Furthermore, even if PMCT could demonstrate ground-glass opacities in non-dependent areas of the overinflated lungs which is consistent with freshwater drowning, it could also be seen in many other instances, including ARDS, pulmonary oedema, interstitial and bronchopneumonia and pulmonary haemorrhages. Therefore, it highlights the fact that VA should not be a substitute, but be used as an adjunct to CA, which is still considered the gold standard.
The use of VA in the investigation of asphyxial deaths is very favourable. VA demonstrates certain limitations in the detailed assessment of aspirated foreign bodies. Although VA using MSCT was able to detect the presence and location of foreign bodies, it fails to identify the type and number of foreign bodies present. 11 This small piece of evidence has great medico-legal significance, which recommends VA to be best used as an adjunct to CA to obtain optimum results in such instances. Furthermore, 39% of false negatives were observed when using PMCT in the investigation of asphyxial deaths proving its limited value in such cases. 29
VA in natural deaths
Although possibly not as useful as in traumatic deaths, VA has proved to be beneficial in some deaths due to natural causes. The detection of structural defects and congenital anomalies leading to death is a crucial aspect of the paediatric population. In this context, VA in combination with CA can be a useful tool in the investigation of deaths in newborns and children with congenital abnormalities.
PM-MRI was performed on newborns to detect innate diaphragmatic hernia and lung hypoplasia where the use of VA enabled a more accurate and objective diagnosis of lung hypoplasia than CA. It was also used for the determination of treatment efficiency of lung conditions in cases of innate diaphragmatic hernia. This shows that PM-MRI can be useful as a less invasive method and an adjunct to CA in the diagnosis of structural heart diseases in paediatric deaths. 31
Malignancies with metastasis in the paediatric population are another instance where VA has been considered a useful adjunct. PM-MRI was successfully employed in the diagnosis of a right adrenal mass with multiple liver metastases in a neonate combined with limited and targeted sampling for histological confirmation of the malignancy.15,16 Furthermore, VA has been useful to identify the primary mass and the extent of metastatic disease. This highlights the usefulness of VA adjunct with limited sampling to arrive at an accurate COD, especially in instances that restrict/prevent the conduct of CA. Although CA is the gold standard, in such instances detection of metastatic malignancies may be better accomplished with VA.
In the assessment of fluid in body cavities, VA proved to be more beneficial than CA. PM-MRI with 3D reconstruction has been successfully used to detect and quantify anasarca in newborns with congenital abnormalities. VA provided a more objective and accurate quantitative assessment of anasarca. This is a challenging task to undertake with CA alone due to the spilling of fluid between tissues and cavities during dissection and the need for additional incisions causing disfigurement. Therefore, VA can be considered as a better method to quantitatively assess anasarca and fluid accumulations in serous cavities in newborns and children PM.
However, VA is not without its pitfalls in the investigation of natural deaths. Differences in the organ-specific sensitivity of VA are observed. Due to the inability to differentiate AM injury from PM changes, the diagnosis of ischaemic brain injury and myocarditis is proven to be problematic.20,30 Furthermore, PM-MRI alone has not proven to be adequate to opine whether the hypoxic–ischemic changes are an agonal manifestation or PM change/artefact.
Furthermore, abdominal and lung pathology detection was poor with PM-MRI except for major structural abnormalities. 30
The diagnostic value of PM-MRI for intra-thoracic pathologies in paediatric PMs is not satisfactory due to the low sensitivity in the detection of non-cardiac thoracic abnormalities, especially pulmonary infections, and pulmonary haemorrhages. 32
PMCT could detect the final COD in only 7 out of 54 cases (12.9%), with the highest incidence of detection in gastrointestinal pathologies. Although PMCT could detect additional, incidental pathologies in 12.9% of cases, in 40 out of 54 cases (74.1%) it did not detect important findings contributing to the final COD. Therefore, the benefits of VA in the investigation of natural deaths appear to be limited. 28
However, regarding abdominal pathologies, in some cases, PM-MRI demonstrated a high sensitivity for renal pathologies, with low diagnostic sensitivity in adrenal, hepatic and intestinal pathologies. 33
PMCT with 3D reconstruction was used to determine (1) gestational age, (2) live versus stillbirth and (3) the COD in decomposed bodies of newborns. Although the estimation of gestational age is better with PMCT using long bone measurements, neither CA nor PMCT was able to determine a reliable COD due to advanced decomposition. 19
Regarding the system-specific usefulness of VA, PM-MRI is in total agreement with the clinical COD in 19 out of 31 cases (61%), especially in cardiovascular and hepatic pathologies. However, in 7 out of 31 cases (22%), VA was unable to match the clinical COD. 25 Furthermore, VA appears to be superior to CA in detecting free air in thoracic and peritoneal cavities and hepatic iron overload. However, CA has been superior to PM-MRI in detecting focal bowel necrosis and perforation, focal pulmonary haemorrhage and consolidation, medial hypertrophy in the pulmonary vascular bed, microscopic changes of acute tubular necrosis, focal microscopic white matter injury and hypoxic-ischemic injury.
When considering the sensitivity of different modalities of VA for detecting organ pathologies, a higher detection rate was observed with PM-MRI for abdominal, cardiac and neurological pathologies, whereas with PMCT for chest pathologies. The detection of musculoskeletal pathologies was equal for both methods. 24 However, the overall sensitivity for paediatric pathologies is higher for PM-MRI compared to PMCT, whereas PMCT has shown a higher specificity.
There can be instances where VA should be used with extreme caution to avoid misinterpretations that can lead to erroneous conclusions. 26 In PMCT images, significant focal tapering at the arch of the aorta between the origin of the brachio-cephalic artery and the left subclavian artery has been observed. This can be identified as a PM change and can easily be misinterpreted as a hypoplastic aortic arch. 26 Such misinterpretation of PM artefacts/changes through VA would lead to wrongful COD. This highlights the counter-beneficial effects of VA on the final COD.
Another significant limitation in the application of VA in routine practice is the requirement for specialized training and expertise to get the maximum benefit from VA. 17 This is vital to minimize over-interpretation of non-specific findings, consistent with PM changes and resuscitation artefacts, that do not add to the COD, thereby reducing the number of false positives leading to inaccurate diagnosis and wasted resources.
The ability to detect cardiac pathologies through PMCT is poor in some studies due to various factors. The reasons include poor resolution of PMCT for cardiac structures, PM clotting, intracardiac gas, absence of contrast agent and collapsed cavities.23,27 Detection of pulmonary pathologies was also found to be sub-optimal with PMCT, with poor detection of aspirated material and differentiation of AM and PM lesions. Furthermore, PMCT did not differentiate AM pulmonary manifestations of heart failure, aspiration pneumonia and infection from non-specific agonal and/or PM changes. Therefore, non-contrast PMCT is not useful in the detection of lesions in organ parenchyma and soft tissues. However, these limitations can be circumvented to a certain extent using PM-MRI and contrast enhancement. On the whole, it can be concluded that CA is better than VA in detecting pathologies in organ parenchyma, soft tissues and the vascular system.
In some instances, PM-MRI has failed to detect hypoplasia of the ductus venosus, pneumonia, candida and cytomegalovirus infection, atrial septal defect and papillary muscle infarction. 29 This also confirms that CA is the gold-standard in death investigation, and therefore should not be completely substituted by VA.
Therefore, it is mandatory for clinicians and pathologists to be aware of the importance of CA and the limitations of VA. Thus, the employment of VA should be decided case-by-case by the forensic pathologist taking into consideration all the benefits and pitfalls.
VA in postoperative deaths
The use of VA in postoperative deaths was highlighted in some instances. For example, PMCT angiography in cases with postoperative fatal haemorrhage appears to be crucial and superior to CA in detecting the point of bleeding. 13
VA in unascertained deaths
The COD was unascertained in 36 cases discussed in the reviewed articles. The combined use of CA, VA and other ancillary investigations including histology and toxicology has satisfactorily formulated a COD in any of the cases.
Limitations
Selection bias is a major limitation in this study as grey literature with undeniable value may have been undetected. And the heterogeneity of the included articles with regard to the methodology poses a risk of bias and limited standardization.
Conclusion
In the investigation of unnatural deaths, VA is more accurate and objective than CA in the detection of skeletal trauma, bullet trajectory and quantification of air/fluid in body cavities. VA is beneficial especially in the context of NAIs to exclude child abuse. However, in asphyxial deaths, stillbirths and decomposed bodies, VA is best used as an adjunct to CA.
In the investigation of natural deaths, the use of VA is disease-specific and organ-specific. VA is better at detecting structural/congenital abnormalities; therefore, it is more advantageous in the paediatric population compared to adults. However, VA has limited value in differentiating AM and PM changes with the added risk of gross misinterpretations.
Therefore, the use of VA in the investigation of deaths in the paediatric population should be tailored to the circumstance and mechanism of death to gain the best outcome.
Supplemental Material
sj-docx-1-smo-10.1177_20503121231172002 – Supplemental material for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review
Click here for additional data file. (12.7KB, docx)
Supplemental material, sj-docx-1-smo-10.1177_20503121231172002 for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review by Chathula Wickramasinghe, Deepthi Edussuriya, Sriyani Perera and Nimashi Herath in SAGE Open Medicine
sj-pdf-1-smo-10.1177_20503121231172002 – Supplemental material for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review
Click here for additional data file. (80.7KB, pdf)
Supplemental material, sj-pdf-1-smo-10.1177_20503121231172002 for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review by Chathula Wickramasinghe, Deepthi Edussuriya, Sriyani Perera and Nimashi Herath in SAGE Open Medicine
Footnotes
Author contributions: All authors substantially contributed to the outcome of this systematic review. CUW and DE conceived the study. All authors developed the study protocol. A systematic and comprehensive search was conducted by SP. DE and CUW independently screened the uploaded articles in Rayyan and independently assessed the quality of the selected studies. Data extraction was done by CUW and NH. A narrative synthesis of the findings from individual included studies was carried out by DE and CUW. All authors contributed to the drafting and revising of the manuscript and have approved the content of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Study registration: This study was registered in the PROSPERO registry (CRD42021236545).
ORCID iD: Chathula Ushari Wickramasinghe

Availability of data and materials: Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Supplemental material: Supplemental material for this article is available online.
References
1.Ahmad M, Rahman FN. Virtual autopsy: a new trend in forensic investigation. J Armed Forces Med Coll Bangladesh 2013; 9(2): 100–106. [Google Scholar]
2.Rizzo A. Autopsy and religion: aiding forensics, medicine, and families with the virtual autopsy. J Emerging Forensic Sci Res 2019; 4(1): 31–42. [Google Scholar]
3.Malizia A, Filograna L, Ryan CP, et al. Post-mortem investigation through virtual autopsy techniques: proposal of a new diagnostic approach to reduce the risks of operators during emergencies. Int J Saf Secur Eng 2020; 10(4): 535–541. [Google Scholar]
4.Okuda T, Shiotani S, Sakamoto N, et al. Background and current status of postmortem imaging in Japan: short history of “Autopsy imaging (Ai)”. Forensic Sci Int 2013; 225(1–3): 3–8. [DOI] [PubMed] [Google Scholar]
5.Arthurs OJ, van Rijn RR, Taylor AM, et al. Paediatric and perinatal postmortem imaging: the need for a subspecialty approach. Pediatr Radiol 2015; 45(4): 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
6.Vadivel JK. Virtual autopsy. Int J Forensic Odontol 2016; 1(1): 14–16. [Google Scholar]
7.Moher D, Shamseer L, Clarke M, et al.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Sys rev 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
8.Eden J, Levit L, Berg A, et al. Finding what works in health care: standards for systematic reviews. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
9.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst rev 2016; 5(1): 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
10.The Joanna Briggs Institute. Checklist for studies of multiple designs of the Joanna Briggs Institute Critical Appraisal tools for use in systematic reviews. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Systematic_Reviews2017_0.pdf (2017, accessed 10 June 2022).
11.Rutty GN, Jeffery AJ, Raj V, et al. The use of post-mortem computed tomography in the investigation of intentional neonatal upper airway obstruction: an illustrated case. Int J Legal Med 2010; 124(6): 641–615. [DOI] [PubMed] [Google Scholar]
12.Ebert LC, Schön CA, Ruder TD, et al. Fatal left ventricular rupture and pericardial tamponade following a horse kick to the chest. Am J Forensic Med Pathol 2012; 33(2): 167–169. [DOI] [PubMed] [Google Scholar]
13.do Nascimento FB, dos Santos GA, Melo NA, et al. Detection of the source of hemorrhage using postmortem computerized tomographic angiography in a case of a giant juvenile nasopharyngeal angiofibroma after surgical treatment. Forensic Sci Med Pathol 2015; 11(3): 427–431. [DOI] [PubMed] [Google Scholar]
14.Filograna L, Tartaglione T, Vetrugno G, et al. Freshwater drowning in a child: a case study demonstrating the role of post-mortem computed tomography. Med Sci Law 2015; 55(4): 304–311. [DOI] [PubMed] [Google Scholar]
15.Davis J, Novotny N, Macknis J, et al. Diagnosis of neonatal neuroblastoma with postmortem magnetic resonance imaging. Radiol Case Rep 2017; 12(1): 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
16.Andronikou S, Kemp ML, Meiring M. Whole-body MRI virtual autopsy using diffusion-weighted imaging with background suppression (DWIBS) at 3 T in a child succumbing to chordoma. J Pediatr Hematol Oncol 2017; 39(2): 133–136. [DOI] [PubMed] [Google Scholar]
17.Harty MP, Harcke HT, Gould SW, et al. Pulmonary embolus as cause of death in an adolescent: demonstration on postmortem CT. Pediatr Radiol 2018; 48(5): 745–748. [DOI] [PubMed] [Google Scholar]
18.Del Fante Z, De Matteis A, Fazio V, et al. The importance of postmortem computed tomography (PMCT) in the reconstruction of the bullet trajectory. Clin Ter 2019; 170(2): 129–133. [DOI] [PubMed] [Google Scholar]
19.Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, Maes A, et al. The value of post-mortem CT in neonaticide in case of severe decomposition: description of 12 cases. Forensic Sci Int 2013; 233(1–3): 298–303. [DOI] [PubMed] [Google Scholar]
20.Montaldo P, Chaban B, Lally PJ, et al. Quantification of ante-mortem hypoxic ischemic brain injury by post-mortem cerebral magnetic resonance imaging in neonatal encephalopathy. Eur J Paediatr Neurol 2015; 19(6): 665–671. [DOI] [PubMed] [Google Scholar]
21.Tumanova UN, Lyapin VM, Bychenko VG, et al. Possibilities of postmortem magnetic resonance imaging for evaluation of anasarca in Newborns. Bull Exp Biol Med 2019; 166(5): 671–675. [DOI] [PubMed] [Google Scholar]
22.Tumanova UN, Lyapin VM, Burov AA, et al. The possibility of postmortem magnetic resonance imaging for the diagnostics of lung hypoplasia. Bull Exp Biol Med 2018; 165(2): 288–291. [DOI] [PubMed] [Google Scholar]
23.Krentz BV, Alamo L, Grimm J, et al. Performance of post-mortem CT compared to autopsy in children. Int J Legal Med 2016; 130(4): 1089–1099. [DOI] [PubMed] [Google Scholar]
24.Arthurs OJ, Guy A, Thayyil S, et al. Comparison of diagnostic performance for perinatal and paediatric post-mortem imaging: CT versus MRI. Eur Radiol 2015; 26(7): 2327–2336. [DOI] [PubMed] [Google Scholar]
25.Leadbetter KZ, Vesoulis ZA, White FV, et al. The role of post-mortem MRI in the neonatal intensive care unit. J Perinatol 2017; 37(1): 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
26.Simanovsky N, Hiller N, Timofeev M, et al. Postmortem computer tomography appearance of the aortic arch in children: what is considered normal?. Isr Med Assoc J 2017; 19(10): 640–643. [PubMed] [Google Scholar]
27.Proisy M, Marchand AJ, Loget P, et al. Whole-body post-mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 2013; 23(6): 1711–1719. [DOI] [PubMed] [Google Scholar]
28.Rijn RRV, Beek EJ, van de Putte EM, et al. The value of postmortem computed tomography in paediatric natural cause of death: a Dutch observational study. Pediatr Radiol 2017; 47(11): 1514–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
29.Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, de Bakker H, et al. Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 2014; 128(6): 957–965. [DOI] [PubMed] [Google Scholar]
30.Thayyil S, Sebire NJ, Chitty LS, et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 2013; 382(9888): 223–233. [DOI] [PubMed] [Google Scholar]
31.Taylor AM, Sebire NJ, Ashworth MT, et al. Postmortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation 2014; 129(19): 1937–1944. [DOI] [PubMed] [Google Scholar]
32.Arthurs OJ, Thayyil S, Olsen OE, et al. Diagnostic accuracy of post-mortem MRI for thoracic abnormalities in fetuses and children. Eur Radiol 2014; 24(11): 2876–2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
33.Arthurs OJ, Thayyil S, Owens CM, et al. Diagnostic accuracy of postmortem MRI for abdominal abnormalities in foetuses and children. Eur J Radiol 2015; 84(3): 474–481. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
sj-docx-1-smo-10.1177_20503121231172002 – Supplemental material for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review
Click here for additional data file. (12.7KB, docx)
Supplemental material, sj-docx-1-smo-10.1177_20503121231172002 for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review by Chathula Wickramasinghe, Deepthi Edussuriya, Sriyani Perera and Nimashi Herath in SAGE Open Medicine
sj-pdf-1-smo-10.1177_20503121231172002 – Supplemental material for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review
Click here for additional data file. (80.7KB, pdf)
Supplemental material, sj-pdf-1-smo-10.1177_20503121231172002 for Usefulness of virtual autopsy in diagnosing pathologies in the paediatric population: A systematic review by Chathula Wickramasinghe, Deepthi Edussuriya, Sriyani Perera and Nimashi Herath in SAGE Open Medicine
Articles from SAGE Open Medicine are provided here courtesy of SAGE Publications
Like this project
Posted Feb 12, 2025
Virtual autopsy is a non-invasive/minimally invasive method for conducting an autopsy, with the assistance of imaging techniques. We aim to review the benefits…
Likes
0
Views
1