Healthcare Provider Fraud Detection
Like this project
Posted Sep 7, 2025
Developed a machine learning model to detect healthcare fraud with improved recall and precision.
Likes
0
Views
0
Timeline
Jul 2, 2025 - Jul 31, 2025
Healthcare Provider Fraud Detection
Project Overview
This project aims to develop a robust machine learning solution for detecting potential fraudulent activities among healthcare providers. Healthcare fraud poses a significant financial burden on insurance systems and governments, diverting resources and compromising patient care. This initiative leverages machine learning to proactively identify suspicious patterns in claims and beneficiary data, enabling targeted investigations and mitigating financial losses.
Problem Statement
The core challenge addressed is the accurate identification of fraudulent providers within a highly imbalanced dataset, where fraudulent cases are rare. The primary objective is to build a model that maximizes Recall – the ability to correctly identify as many actual fraudulent providers as possible – without an excessive compromise to Precision – minimizing the number of legitimate providers incorrectly flagged as fraudulent, which can lead to inefficient investigations.
Dataset
The project utilizes a simulated healthcare claims dataset, structured across multiple interconnected CSV files, for both training and unseen prediction:
Training Data Set
Train_Beneficiarydata-1542865627584.csv: Contains demographic and health-related information for various beneficiaries (e.g., BeneID, Age, Gender, ChronicCond_*).Train_Inpatientdata-1542865627584.csv: Records of inpatient claims, including details like ClaimID, Provider, AttendingPhysician, AdmissionDt, DischargeDt, ClmDiagnosisCode_*, ClmProcedureCode_*, InscClaimAmtReimbursed, and DeductibleAmtPaid.Train_Outpatientdata-1542865627584.csv: Similar to inpatient data but for outpatient claims.Train-1542865627584.csv: The target file containing Provider IDs and their corresponding PotentialFraud status ('Yes' or 'No').Test/Unseen Data Set
Unseen_Beneficiarydata-1542969243754.csvUnseen_Inpatientdata-1542969243754.csvUnseen_Outpatientdata-1542969243754.csvUnseen-1542969243754.csv: Contains Provider IDs for which fraud predictions are to be submitted.Project Goals
Develop a Robust Predictive Model: Build a machine learning model capable of accurately classifying healthcare providers as fraudulent or non-fraudulent.
Optimize for Recall: Enhance the model's ability to identify actual fraud cases (high recall) while maintaining an acceptable level of precision.
Generate Predictions: Apply the trained model to unseen data and provide a submission file with predicted fraud probabilities and classes.
Provide Actionable Recommendations: Offer business-oriented insights and strategies for utilizing the model and for future improvements in fraud detection.
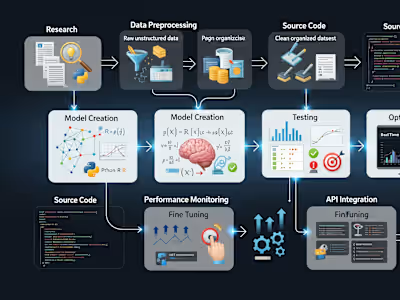
Methodology and Approach
The project followed a comprehensive machine learning pipeline, emphasizing data preparation, feature engineering, advanced modeling, and rigorous evaluation.
1. Data Management and Preprocessing
Data Loading: All training and unseen datasets were loaded using Pandas.
Data Merging:
Inpatient and Outpatient claims were combined into a single claims dataset.
This combined claims data was then merged with the beneficiary data (
BeneID) to enrich claim records with beneficiary demographics and chronic conditions.Finally, this merged claims-beneficiary data was linked to the
Train.csv (or Unseen.csv) file based on Provider ID, which served as the aggregation key and target identifier.Initial Cleaning: Ensured data types were appropriate for numerical operations and date fields were correctly parsed.
2. Feature Engineering
The core of the model's predictive power lies in aggregated and engineered features at the Provider level. This transformation captures behavioral patterns indicative of fraud.
Aggregated Features:
Counts of total claims, inpatient claims, and outpatient claims (
TotalClaims, TotalInpatientClaims, TotalOutpatientClaims).Sum and average of reimbursed amounts and deductible paid (
SumInscClaimAmtReimbursed, AvgInscClaimAmtReimbursed, SumDeductibleAmtPaid, AvgDeductibleAmtPaid).Average demographic and health indicators of beneficiaries associated with the provider (
AvgAge, AvgGender, AvgRace, AvgChronicCond_*, AvgRenalDiseaseIndicator).Counts of unique beneficiaries, attending, operating, and other physicians (
UniqueBeneIDs, UniqueAttendingPhysicians, UniqueOperatingPhysicians, UniqueOtherPhysicians).Counts of unique diagnosis and procedure codes (
UniqueClmDiagnosisCode_*, UniqueClmProcedureCode_*, UniqueClmAdmitDiagnosisCode, UniqueDiagnosisGroupCode).Average claim duration (
AvgClaimDuration) and average inpatient stay duration (AvgInpatientStayDuration).Proportion of claims with missing physician information (
PropMissingAttendingPhysician, PropMissingOperatingPhysician, PropMissingOtherPhysician).Advanced, Domain-Specific Features: These were engineered to capture more subtle fraud indicators:
ClaimsWithManyDiagnosisCodes: Counts claims with at least 4 diagnosis codes, potentially signaling 'upcoding' or unnecessary complexity.InpatientToOutpatientRatio: The ratio of inpatient to outpatient claims, which can reveal unusual service distribution by a provider.ReimburseToDeductibleRatio: The ratio of total reimbursed amount to total deductible paid, flagging abnormal financial patterns.PropClaimsWithOperatingPhysician: Proportion of claims where an operating physician is listed, which might indicate higher volumes of complex or invasive procedures.Missing Value Handling: Missing values, particularly those resulting from aggregations where a certain type of claim/data was absent for a provider (e.g.,
AvgInpatientStayDuration for providers with no inpatient claims), were imputed using the median value of their respective columns.3. Modelling and Evaluation
The problem was treated as a binary classification task. Due to the inherent class imbalance (fewer fraudulent providers), specific strategies were employed.
Baseline Model: Random Forest Classifier
An initial Random Forest model was trained to establish a performance baseline. While it showed high overall accuracy and decent precision, its recall (51%) was relatively low, indicating a significant number of fraudulent providers were being missed.
Optimization 1: Threshold Tuning for Random Forest
To address the low recall, the classification threshold for the Random Forest model's predicted probabilities was tuned. By lowering the threshold from the default 0.5, the model became more sensitive to the positive class (fraud).
Result: This successfully boosted Recall to 67.33% while maintaining a reasonable precision (64.76%) and an improved F1-score (0.6602).
Optimization 2: XGBoost Classifier
XGBoost, a powerful gradient boosting framework, was chosen for its superior performance, ability to handle complex relationships, and built-in mechanisms for class imbalance.
The
scale_pos_weight parameter was used during training to give more weight to the minority class (fraud), directly addressing the imbalance.Threshold Tuning for XGBoost: Similar to Random Forest, the classification threshold for XGBoost was further optimized to maximize the F1-score, providing the best balance.
Performance Summary
The table below summarizes the performance metrics across different model iterations:
Metric Initial RF RF (Tuned Thresh) XGBoost (Default Thresh) XGBoost (Tuned Thresh) Accuracy 0.9400 0.9353 0.9335 0.9344 Precision 0.7700 0.6476 0.6261 0.6293 Recall 0.5100 0.6733 0.7129 0.7228 F1-Score 0.6200 0.6602 0.6667 0.6728 ROC AUC Score 0.9480 0.9488 0.9495 0.9495
Conclusion: The XGBoost Classifier with a tuned threshold of approximately 0.4986 achieved the best overall performance, significantly increasing the recall to 72.28% while maintaining a precision of 62.93% and a high F1-Score of 0.6728. This model effectively balances the trade-off, enabling the identification of a large proportion of fraudulent providers for investigation.
How to Run the Project
To execute this project and generate predictions on unseen data, follow these steps:
Prerequisites
Ensure you have Python 3.x installed along with the following libraries:
pandas (for data manipulation)numpy (for numerical operations)scikit-learn (for machine learning utilities and metrics)xgboost (for the final model)matplotlib (for plotting)seaborn (for enhanced visualizations)joblib (for saving and loading models)You can install these libraries using pip: