Why Data Without Decisions Creates Anxiety
Monitoring Without Targets: Why Data Without Decisions Creates Anxiety
Patients are often advised to “monitor their readings and adjust accordingly.”
Clinically, this advice is accurate.
Behaviourally, it is incomplete.
Without clear targets, timeframes, and escalation criteria, monitoring turns into guessing — and guessing turns into anxiety.
This case study explores a common scenario in diabetes self-monitoring to show how decision-led guidance transforms the same data into safer behaviour, reduced over-monitoring, and clearer escalation.
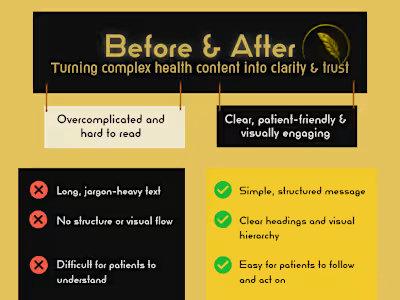
The communication problem
Patients are frequently told:
– “Check your blood glucose before and after meals.”
– “Adjust your diet accordingly.”
– “We’ll review your readings at your next appointment.”
While clinically sound, this advice lacks decision structure.
Patients are left unsure what matters now, what can safely wait, and what should trigger action.
What’s actually missing
The issue isn’t lack of information.
It’s lack of decision structure.
Patients aren’t unsure because they lack data.
They’re unsure because they don’t know:
– what matters now
– what can safely wait
– what would change the plan
Information without structure forces people to guess.
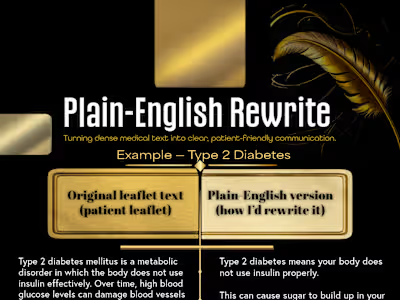
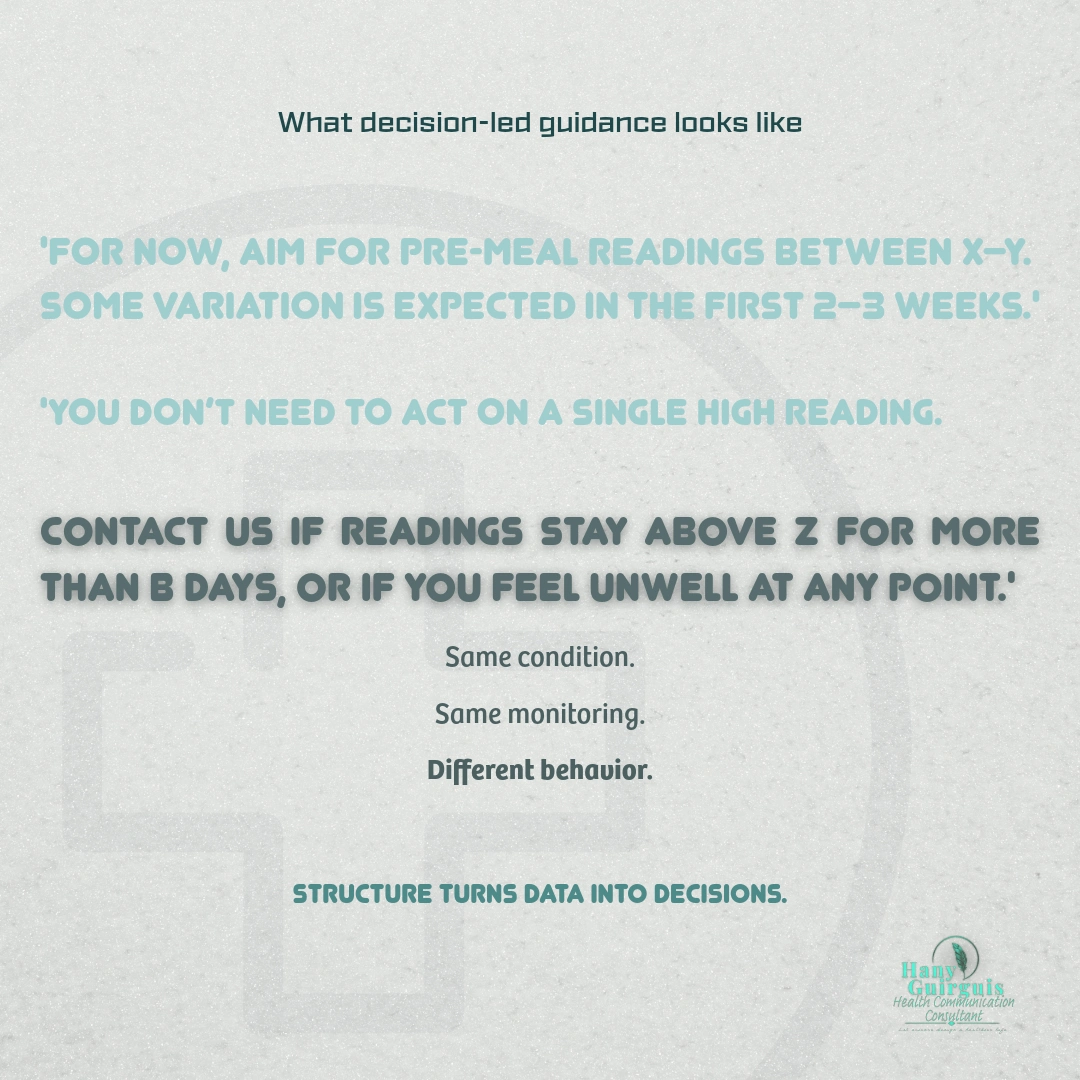
What decision-led guidance looks like
Decision-led guidance turns monitoring into action by clarifying:
– target ranges
– expected variation
– timeframes for review
– clear escalation triggers
For example:
“For now, aim for pre-meal readings between X–Y.
Some variation is expected in the first 2–3 weeks.
You don’t need to act on a single high reading.
Contact us if readings stay above Z for more than B days, or if you feel unwell at any point.”
Why this reduces risk
Decision-led guidance:
– reduces unnecessary monitoring
– normalises expected variation
– encourages timely escalation
– supports patient confidence and wellbeing
Clarity is not reassurance.
Clarity is a safety intervention.
My role
Clinical Pharmacist and Health Communication Consultant
I apply NHS-style plain English, safety-netting, and behavioural insight to translate clinical accuracy into patient-safe action.
Like this project
Posted Jan 11, 2026
A clinical communication pattern showing how unclear monitoring advice increases patient anxiety — and how decision-led guidance reduces risk.
Likes
0
Views
0