Inventing the Future of Sleep Medicine
Like this project
Posted Aug 6, 2023
Using the Eye-Comtm Biosensor, Communicator and Controller eye-tracking system, developed by William Torch, MD, researchers are gaining insights into yet anoth…
Likes
0
Views
0
Sleep professionals at Washoe Sleep Disorders Center are exploring how sleep deprivation affects cognitive abilities andneurological disorders. Using the Eye-Comtm Biosensor, Communicator and Controller eye-tracking system, developed by William Torch, MD, researchers are gaining insights into yet another fertile area of sleep research.
Heart and lung specialists have increasingly focused on the consequences of poor sleep, but what about brain researchers? For neurologist William Torch, MD, the sleep/brain connection is a chief area of concern, and that interest has simmered since the early days of sleep medicine.
When Torch came from New York City to Nevada in 1979 to join the Pediatrics Department at the University of Nevada School of Medicine in Reno, he became the Silver State’s first pediatric neurologist. In addition to his MD from the University of Rochester School of Medicine, he brought credentials as a researcher with an MS degree in biochemistry.
EVOLUTION OF A SLEEP DOCTOR
During his neurology residency in 1974, Torch met Dr Elliott Weitzman, chairman of neurology at the Albert Einstein College of Medicine, sparking a lifelong dedication to sleep medicine research. Torch had always been intrigued with the curious EEG brain waves associated with pediatric and adult sleep states, especially Weitzman’s pioneering research on rapid eye movement (REM) and the mysteries of sleep neurophysiology, also being explored by Dr William Dement at Stanford University.
At the time, sleep medicine was a “dark science” and few doctors recognized the importance of sleep in daytime functions. From that point on, Torch and sleep medicine would unwittingly cross paths, resulting in many research innovations. Once settled in Nevada, Torch started the Neuro-Developmental & Neuro-Diagnostic Center (NDC) as a multidisciplinary clinic treating neurological disorders, and performing regular and 24-hour ambulatory and quantitative EEGs on children and adults with attention deficit disorder (ADD), epilepsy, sleep, and other neuropsychiatric disturbances, while also serving as the medical director of the Northern Nevada Muscular Dystrophy Association clinic.
Torch and sleep medicine began traveling the same path after a fortuitous 1984 meeting with experimental psychologist Dr John Zimmerman, who had previously worked in a Colorado sleep lab. When Zimmerman offered to start the first sleep disorders clinic in Reno, Torch agreed, and the Washoe Sleep Disorders Center (WSDC) was born. The venture brought sleep medicine and neurology under one roof, while laying the groundwork for Eye-Com Corporation (ECC) in 1998.
EC-1
HUMBLE BEGINNINGS
Torch and Zimmerman started the WSDC from scratch with the support of the Washoe Medical Center, which provided space for a one-bed sleep lab. Together, they built their own primitive sleep recording polysomnographic equipment, attaching a camera to a makeshift paper tracing EEG machine that they lugged around the hospital, while performing less than five inpatient polysomnograms (PSGs) each month. “It was an expensive joke,” Torch says, and “when we started a sleep medicine grand rounds teaching program, we also found that no one believed in sleep medicine as a discipline, and only a few would come.”
Nevertheless, after 3 years the lab was performing about five to 10 inpatient sleep studies per month. By 1994, the WSDC had grown into a two-bed lab performing 20 to 30 inpatient and outpatient sleep studies each month.
Soon afterwards, it received its first 5-year accreditation from the American Academy of Sleep Medicine (AASM), with three more 5-year reaccreditations to come. Torch finally moved the NDC/WSDC into its new four-bed facility in the Renown Center for Advanced Medicine, while gradually expanding its staff of two to 12, including the Lab Director, Dr Paul Saskin, six board-certified sleep and EEG technicians, and two nurse practitioners. The NDC/WSDC now accommodates more than 400 patient visits and performs 70 to 90 sleep studies each month, with expectations of doubling in size over the next 2 years. In recognition of his Nevada accomplishments, Torch was elected as the first president of the AASM-sponsored Nevada Sleep Society.
EVOLUTION OF AN INVENTOR
EC-4
Torch wears three hats as a clinician, researcher, and inventor, and he has dreamed up a number of sleep-related inventions during his own REM sleep. This included the Sleep Managertm—a hardware and software calculating system (soon to become an Apple App), which can help prevent jet lag and shift work fatigue, and the Eye-Comtm Biosensor, Communicator and Controller.
Torch’s goal has always been to deploy new technologies to help neurologically disabled children and adults with progressive neuromuscular disorders such as muscular dystrophy or ALS, as well as more static conditions like cerebral palsy, stroke, and traumatic spinal cord or brain injury, to achieve independence and freedom of movement.
Torch’s vision to help such victims materialized in 1998, when asked to consult on a young man named Glen, who awoke from a coma on a ventilator in an ICU, following a stroke to his cervical spinal cord—the result of viral encephalomyelitis. The condition left him totally quadriplegic. “The only way he could communicate was to move his eyes and blink once or twice in response to yes/no questions … and cry,” Torch says. “The patient was in a near locked-in-state.
“I went down to Radio Shack and bought about $2.50 worth of IR emitter-detectors and electronic components and built a blink detector, now known as Eye-Com 1 (EC-1). I figured that if I could capture the short and long blinks of this unfortunate fellow, convert them into computerized Morse code dots and dashes, and then into text on a computer, this would give him the gift of communication with loved ones and caretakers. Thus, the passion to develop the Eye-Com as a Biosensor, Communicator and Controller stepped out of my neurology practice.”
After creating the EC-1 “blinkometer,” Torch realized that the simple device that helped Glen could be modified to help other paralyzed individuals with different degrees of disability as well, and at the same time it could be used to identify the long and short blinks and other oculometrics associated with drowsiness and microsleeps for use in transportation and industrial safety applications.
REINVENTING SAFETY BEHIND THE WHEEL
William Torch, MD, wearing EC-7/8
EC-1 incrementally evolved through a series of progressive EC-2 through EC-7/8 iterations, as a Biosensor, Communication and Controller device and technology, to its current to-be-commercialized EC-8 HawkEye Model. Torch’s passion for invention, and love for teaching, won the respect of his colleagues in the Nevada Inventors Association (NIA), and he was soon elected as NIA vice president, and then president.
While NIA president, his EC-4 system was featured in Forbes ASAP, in an article titled “The Inventor Next Door.” Because of the Eye-Com research he had been doing, he was then invited to a “New Technologies in Driver Vigilance Conference” sponsored by the American Trucking Association (ATA) and US Department of Transportation (USDOT) in Washington, DC. By that time, EC-4 had evolved to the point that it could transmit drowsy blink signals through walls by RF telephonic and satellite connections, trigger local audible alarms for emergency responses, as well as connect by wired or wireless connection with EEG and PSG machines in the vicinity, or to remote receiving or monitoring stations 3,000 miles away, as it did in Cambridge, Mass, by setting off eye-blink triggered Lifeline alarms at that site. Operating as a drowsiness detector that could alert a sleepy driver, EC-4 could also, as a communication-controller device, be used to type messages on a computer screen by purposeful eye blinks.
Torch brought his EC-4 to the conference where he was first introduced to the term “PERCLOS,” an acronym for the percentage of time one’s eyes are closed over a period of time. Torch instantly realized that he had, without awareness, already created a wearable, wireless PERCLOS-monitoring eye-blink Biosensor, Communicator and Controller. The PERCLOS algorithm had been developed by other researchers in the sleep and transportation safety field, out of video analysis of a sleepy driver’s eyes in a research driving simulator. Soon thereafter, the PERCLOS metric was announced by the USDOT as the best bio-physiological measure of drowsiness available, even over EEG, Torch says.
EC-7
At the conference, Torch met colleague Col Michael Russo, MD, a neurologist who was to become a section chair of the AASM Sleep Deprivation Committee. Russo immediately recognized that Eye-Com technology could contribute to solving the problem of soldier and military truck drivers falling asleep on long truck convoys, as had occurred during Desert Storm operations, or of army helicopter pilots falling asleep at the controls of a multimillion-dollar Black Hawk or Apache helicopter.
After attending the conference, Torch realized that there were other ocular manifestations relating to sleepiness and arousal, where, for example, slow downward lid movements might indicate gradual falling asleep, while a sudden upward eyelid movement might signify an arousal or startled response. He also realized that the rate and diameter size change of a pupil was important as a predictor of progressive drowsiness where, as shown in experimental pupillometry studies, the sleepier you become, the smaller and less reactive your pupil gets over time.
Based on these realizations, Torch went on to develop the EC-5, which could measure PERCLOS and upward and downward lid velocities. Next, by attaching two Eye-Com “micro-endocameras” to an eye-frame, one below and aimed at each eye, and a single “exo-camera” aimed forward from the nasal bridge just above the nose, he could monitor pupils, eyeball movements, and gaze characteristics as well. These were the oculometrics that might be associated with microsleep intrusions, brain fog, and tunnel vision.
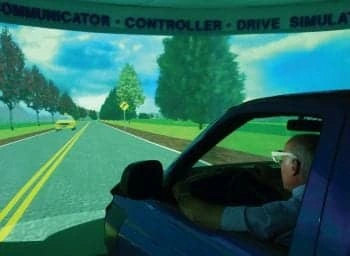
One year later, Torch was invited to another USDOT-sponsored conference on driver vigilance that spurred him to create the “ideal sleep detection and safety response device.” During that 1-year interval, the USDOT had realized the importance of eye movement and gaze, announcing a second follow-up conference called “New Ocular Technologies in Driving Vigilance.” This time the NDC/WSDC and Eye-Com Corporation came, not as a spectator, but as a participant, displaying its ground-breaking technology in a booth next to that of another company, Real Time Technology, which was looking for a device that could trigger their proprietary tactile race-car seat to vibrate a person awake. The match “made in heaven,” Torch says, resulted in an EC-6 vibrating seat that was eventually installed into a Dodge-Ram Eye-Com truck simulator that was built over the next year in the WSDC.
Artistic rendition of EC-9
FUNDING THE FUTURE OF SAFETY
While Torch was serving as NIA president, he also was told of an upcoming Phase I Small Business Innovation Research (SBIR) Solicitation Grant sponsored by the Centers for Disease Control and Prevention (CDC) Division of Accident and Injury Protection. The solicitation called for new technology that could: 1) identify drowsiness; 2) call for emergency assistance for elderly individuals; and 3) assist in the neuro-rehabilitation process of those injured in an accident.
Realizing the “hand-in-glove” fit of EC-6, he applied for the grant, and on what Torch calls a “magical day,” September 10, 2001, he was awarded the $100,000 grant to further develop and validate the Eye-Com 6 for the defined SBIR Tasks. ECC successfully completed the CDC SBIR Phase I Grant within a year, demonstrating that a wired or wireless EC-6 could clearly identify and respond to the drowsy oculometrics of sleep-deprived subjects with sleep apnea or narcolepsy, and normal controls, in a simple desktop computer drive simulator program called Steer Clear.
In that CDC study, it was shown that the PERCLOS measurements of sleepy subjects tested in that 24-hour sleep deprivation study had the same eye characteristics as patients previously diagnosed with ADD and attention-deficit hyperactivity disorder (ADHD). This led to Torch’s conviction that ADD/ADHD may, in many cases, be the “functional expression” of underlying states of sleepiness associated with the growing epidemic of insufficient sleep in the United States—in both the civilian and military worlds. According to military professionals, long hours on duty, and missions associated with sleep deprivation, are the rule—and frequently the cause of irritable or aggressive behavior, road rage, and human factors-related performance-vigilance failures leading to the unwanted consequences of friendly fire and collateral damage, Torch says. With these considerations in mind, the Department of Defense (USDOD) invited the WSDC and ECC to apply for a US Army-sponsored 2003 Phase I $75,000 SBIR Grant, and as before, the two were once again awarded.
During the Phase I study conducted in 2004, ECC refined the EC-6 and developed Eye-Com Eye-Seetm oculometric software that could be used to study the eyes of drivers and pilots in a more advanced desk-top STISIM Drive simulator installed in the WSDC/NDC. It was demonstrated that Eye-Seetm had the potential of tracking more than 30 different eyelid, eyeball, and pupil movements, including PERCLOS, in real time as well as from previously recorded video of an EC-6 wearer’s eyes. During the Army Phase I study, EC-6 was deployed within a full immersion UH-60 Black Hawk helicopter flight simulator at Ft Rucker, Ala, and the US Army Aeromedical Research Laboratory Engineering Directorate approved its use in further real and simulated helicopter studies.
Upon completion of Phase I study, Torch, as principal investigator, was invited to apply for a follow-up $750,000 US Army Phase II SBIR Grant to further develop the EC-6 as a Soldier-Mounted Eye-Gaze tracking technology, which could be incorporated into glasses worn under pull-down masks and visors, as well as attached to night-vision scopes and goggles, or physically incorporated into head-mounted displays and scuba masks.
Upon receipt of the award, the WSDC and ECC began to take center stage with a full immersion Eye-Com Drive Simulator within the WSDC. “I brought in a Dodge Ram truck,” Torch says, “sliced it in half, took out the guts, brought the two halves up in an elevator to the seventh floor facility, put it on a wooden frame, built a wrap-around screen around it with three projectors, and integrated the EC-6-Com with other bio-physiological recorders, including EEG, into the Eye-Com Truck Drive Simulator to monitor drowsiness and effects of sleep deprivation on patients with sleep apnea, narcolepsy, and ADD, and normal controls with no sleep disorder.”
During this Institutional Review Board-approved 24- to 36-hour sleep deprivation EC-6 Drive Simulator study, all subjects demonstrated worsening performance in six successive testing sessions, administered every 6 hours, over the 36-hour sleep deprivation period. In each of the six successive sessions, there were progressive increases in EC-6 generated Eye Blink Frequency, Eye Blink Duration, and PERCLOS oculometrics, which correlated with increasing drowsiness and micro-sleeps, along with decreasing attentiveness, increased numbers of errors of omission and commission, and slower reaction times to stimuli, all consistent with ADD/ADHD symptomatology. As in real life, untreated narcoleptic subjects were the most impaired of the four groups, also showing the worst ADD scores.
The Eye-Com COFItm Safety Response Algorithm showing drive simulator accidents as a function of Eye-Com generated PERCLOS oculometrics in subjects with OSA, narcolepsy,and ADD and normal controls, who were tested every 6 hours over a 36-hour sleep deprivation period.
For all groups, EC-6 drowsiness oculometrics were linearly correlated with progressive performance-vigilance decline as documented by proportional increase in drive simulator crashes, center line and road edge excursions, and erratic braking and driving. Circadian changes also were noted, with “second wind” recovery on the sixth testing session for all groups. The findings were consistent with police-reported transportation accident statistics and observations, where most of the simulator accidents occurred in the early morning hours, when driving performance is most impaired in real world driving. Because of its successes under the Federal CDC and US Army’s SBIR Program, ECC and Torch were awarded the coveted National Tibbetts Award in 2006, with further acclaim in the September 2006 Congressional Record. This was followed by receipt of a 2008 Nevada Entrepreneurship Award for Medium Sized Business.
Another EC-6 study funded by the National Highway Traffic Safety Administration Heavy Truck Division of the USDOT and the USDOD included a head-to-head comparison of the wearable EC-6’s PERCLOS-measuring capabilities with Co-Pilot, a dashboard-mounted eye-tracker. The comparative study performed in the Eye-Com Dodge Ram simulator conclusively demonstrated EC-6’s superiority as an unobtrusive wearable eye-frame, which was capable of operating in very demanding environments, as, for example, where the movement of the trucker in a cab might confound a fixed, dashboard-mounted eye-tracker as it loses contact with the driver’s face and eyes, or when the driver is looking away from the dashboard-mounted camera, or wearing obtrusive glasses causing unwanted glints, Torch says.
One of the many innovations to come out of the combined USDOD/USDOT-sponsored study was a new mathematically derived Eye-Com Composite Oculometric Fatigue Index (COFI) and an Eye-Com COFI Safety Response Algorithm, which could trigger audible or tactile alarms of increasing intensity dependent on the degree of sleepiness (eg, mild, moderate, severe) as measured by increasing PERCLOS and longer eye-blink durations associated with drowsiness-impaired driving. The Eye-Com COFI Safety Response now has the potential to be used in the real world to alert a sleepy operator or passengers in the vehicle, to alert surrounding vehicles in danger, or, for that matter, a dispatcher or air controller at a remote monitoring site, to prevent a fatal accident.
A VISION TAKES SHAPE
The EC-6 has evolved into the EC-7 and a futuristic EC-8 to be released this year for Augmentative and Alternative Communication (AAC) applications to help any individual with any degree of disability, whether totally or partially paralyzed. Making all of this possible is EC-7 and EC-8’s newest eye-gaze capabilities, integrating binocular Eye-Com endo-camera eye movement with Eye-Com exo-camera head-pose coordinates, allowing the wearer to control a computer cursor by “point and drag” Eye-Mousetm as well as purposeful eye-blink or eye-dwell functions, which can be used in combination with scalable “click activation” by any functional body part (eg, finger, hand, foot, face, or mouth, etc).
As has already been demonstrated, the EC-7 and future HawkEye EC-8 model, designed to help ALS-afflicted individuals such as Professor Stephen Hawking, will allow users to virtually control any off-the-shelf or specially designed AAC software programs using typing, text, and speech generating keyboards, and an infinite number of software programs.
“Perhaps by reversing the sleep deprivation epidemic that is universal in scope,” Torch says, “we can reverse the unnecessary dependence on stimulants and sleep medications and also drastically reduce the number of near-fatal accidents—the cause of millions of disabling injuries world-wide.”
If you or your company is interested in integrating the Eye-Com technology in your own research applications, or have interest in becoming a beta test site for the new Eye-Com or Sleep Manager technologies, please contact Eye-Com Corporation or William Torch at (775) 329-2006. For more information, please visit the ECC Web site: www.eyecomworld.com.
Tina Page is a freelance writer based in Lomita, Calif. She can be reached at .
William Torch, MD
Washoe Sleep Disorders Center
Renown Center for Advanced Medicine – Building C
75 Pringle Way # 701
Reno, NV 89502
775.329.4060