Understanding Headaches vs. Migraines
Is that Just a Headache or a Migraine Hiding in Plain Sight?
By Oduah Great
7 min read
You wake up with a throbbing head, maybe you skipped breakfast, maybe you didn’t sleep well. You brush it off . “Just a headache.” you say. But what if it isn’t?
Millions of people live with migraines without realizing it, mislabeling them as tension headaches or stress-induced pain. The World Health Organization ranks migraine as the third most prevalent illness in the world, yet it remains one of the most underdiagnosed.
Migraines don’t always announce themselves with flashing lights or severe vomiting. Sometimes, they show up as a dull ache behind one eye, or as unexplained fatigue and irritability the day before the pain hits. That’s why so many people go years without knowing what’s really going on.
Let’s break down the real differences between a regular headache and a migraine , because knowing the truth could change how you treat your pain and your quality of life.
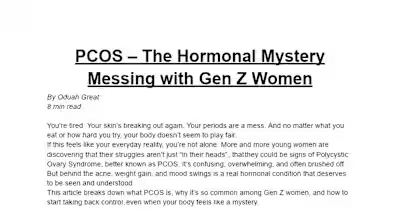
Headaches VS Migraines: What’s the Real Difference?
Many people use the terms headache and migraine interchangeably, but they are not the same. Understanding the differences can help individuals seek the right treatment and avoid prolonged discomfort or complications. Below are some of the key differences:
Pain Quality and Location:
Headaches (especially tension-type headaches) typically cause a dull, constant ache. This pain usually affects both sides of the head and may feel like pressure or tightness, as if a band were wrapped around the skull. In contrast, migraines are characterized by a throbbing or pulsating pain, often localized to one side of the head. This migraine pain is usually more intense and can worsen with routine physical activity or movement (Mayo Clinic).
Duration of Pain:
Tension headaches may last anywhere from 30 minutes to several hours. In most cases, they resolve on their own. Migraine attacks, however, can persist for four to 72 hours if left untreated. They also tend to recur regularly, affecting people multiple times a month or even weekly (American Migraine Foundation).
Presence of Additional Symptoms:
A key distinguishing feature of migraines is the presence of accompanying symptoms. Migraines are commonly associated with nausea, vomiting, and heightened sensitivity to light (photophobia), sound (phonophobia), and sometimes smell. Headaches rarely present with these features (National Institute of Neurological Disorders and Stroke).
Aura and Early Warning Signs:
One-third of people with migraines experience what’s known as an aura-a set of sensory disturbances that precede or accompany the headache. Auras can involve visual effects like flashes of light, zigzag patterns, or blind spots, and may also include numbness, difficulty speaking, or motor weakness. Tension or other common headaches do not present with these neurological warnings (American Academy of Neurology).
Common Triggers
Headaches can be triggered by fatigue, dehydration, skipping meals, or emotional stress. Migraines, on the other hand, have a broader range of potential triggers including hormonal fluctuations (particularly in women), changes in sleep patterns, bright lights, strong odors, weather changes, and certain foods, such as red wine, aged cheese, or chocolate (NHS, WHO).
Impact on Daily Functioning:
While tension headaches are unpleasant, they rarely disrupt daily activities significantly. Migraines can be disabling. Many migraine sufferers are forced to lie down in dark, quiet environments and may miss work or school due to the severity of their symptoms. Chronic migraine, defined as having headache on 15 or more days a month, can have serious implications for a person’s quality of life and mental health (WHO).
The Hidden Impacts of Mislabeling Migraines
Calling every intense headache a migraine (or brushing off a migraine as just a headache) might seem harmless at first. But this common confusion is quietly harming millions. The line between a headache and a migraine isn’t just about language; it determines whether someone receives the right diagnosis, appropriate care, or suffers in silence.
For many, the misunderstanding starts with how we talk about pain. When someone casually refers to any pounding head pain as a migraine, it dilutes the true complexity of the condition. Migraines aren’t simply about head pain. They’re a neurological disorder involving a range of symptoms like visual disturbances, nausea, sensory sensitivity, and sometimes even temporary paralysis. Despite this, over half of people who live with migraines remain undiagnosed (according to the American Migraine Foundation). Without that diagnosis, they often don’t receive preventive treatment or even know such treatment exists.
Instead, many people cycle through over-the-counter painkillers like paracetamol or ibuprofen. But when these are taken several times a week without medical supervision, they can backfire. This pattern can lead to what’s known as ‘medication overuse headaches’ a cruel twist where the very pills meant to help end up perpetuating the pain. It’s a vicious cycle, and one that’s more common than most realize (as noted by the National Institute of Neurological Disorders and Stroke).
Beyond the physical, there’s a deeper emotional cost. Because migraines are often misunderstood or minimized, those who suffer from them can feel invisible (even gaslit). Imagine trying to explain your condition, only to be told, “it’s just a headache” or “you’re being dramatic.” This lack of validation chips away at mental health, contributing to rising rates of depression and anxiety among migraine patients. The internalized doubt and isolation can be as debilitating as the migraine itself.
The consequences extend into the workplace too. When employers view migraines as no different from the average headache, they often fail to provide flexibility or accommodations. Yet globally, migraines are among the leading causes of productivity loss. The World Health Organization ranks them as one of the top ten most disabling conditions (comparable to chronic diseases far more visible in the public eye).
There’s also a wider ripple effect. This confusion affects funding, research, and awareness campaigns. When a condition is poorly understood, it’s less likely to receive the attention it deserves from policymakers or the public. Mislabeling doesn’t just hurt individuals, it holds back progress for everyone living with this often-invisible illness.
Management and Treatment Options
Managing migraines starts with recognizing that each person experiences them differently. This means treatment must be personalized. Before beginning any treatment, it is important to get a proper diagnosis to understand the specific nature of the migraine.
One of the first steps in managing migraines involves making lifestyle changes. Many people find that certain habits or environmental factors can trigger their headaches. These might include irregular sleep schedules, skipping meals, hormonal changes, dehydration, too much caffeine or sudden caffeine withdrawal, bright lights, loud noises, or certain foods like processed meats, aged cheese, or red wine. Keeping a migraine diary can help track patterns by noting daily activities, diet, sleep, and symptoms. This can reveal personal triggers to avoid or manage.
When a migraine attack occurs, acute medications are commonly used to relieve symptoms. Over-the-counter painkillers such as ibuprofen or naproxen work for some. However, moderate to severe migraines often require migraine-specific drugs known as triptans. These medications reduce inflammation and block pain signals in the brain. For those who cannot tolerate triptans, newer options like ditans and gepants have shown effectiveness.
For individuals experiencing frequent migraines, daily preventive treatments may be recommended. These include medications such as beta blockers, certain antidepressants, anticonvulsants like topiramate, or newer therapies targeting a protein called CGRP, which plays a role in migraine development. Preventive treatments aim to reduce the number and severity of migraine attacks rather than stopping them completely.
Non-drug therapies are valuable additions to migraine management. Cognitive behavioral therapy helps improve coping skills and reduce migraine frequency by addressing stress and anxiety. Techniques such as biofeedback, acupuncture, and physical therapy may relieve muscle tension and other related symptoms.
Some patients turn to neuromodulation devices that use electrical or magnetic stimulation to disrupt migraine signals in the nervous system. These FDA-approved devices, such as Cefaly and gammaCore, offer drug-free alternatives and can be helpful, especially for those who experience medication side effects or overuse.
In addition, certain supplements like magnesium, riboflavin (vitamin B2), and coenzyme Q10 have been shown in studies to provide mild preventive benefits. Maintaining regular hydration, engaging in moderate exercise, practicing mindfulness, and incorporating gentle activities such as yoga can also support overall migraine management.
When migraines become chronic or complicated, consulting a neurologist or headache specialist is essential. These experts can customize treatment plans, conduct necessary tests, and help with less common types of migraines.
Migraines can be challenging, but understanding your options is the first step toward relief. With the right care and lifestyle adjustments, it’s possible to take control and improve your quality of life. Remember, help is available, don’t hesitate to reach out to a healthcare professional.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Consult a healthcare provider for diagnosis and treatment tailored to your needs.
References
Like this project
Posted May 17, 2025
Article explaining differences between headaches and migraines.
Likes
0
Views
0