Endocarditis in Intravenous Drug Users: A Dangerous Infection
By Matt Olszewski
Endocarditis infects and inflames the heart’s inner lining and compromises heart valves, often requiring repair or replacement. In the past, rheumatic fever or a congenital defect could be identified as the infective culprit. With IV drug use at an all-time high today, endocarditis cases from infectious needles continue to rise.
The heart pumps over one gallon of blood per minute, delivering oxygen and other nutrients throughout the body. Endocarditis is a potentially fatal infection of the heart's inner lining, which affects valves. With IV drug use on the rise, the prevalence of endocarditis is steadily increasing. Here are some important details on the causes of endocarditis and how to recognize it.
What causes endocarditis?
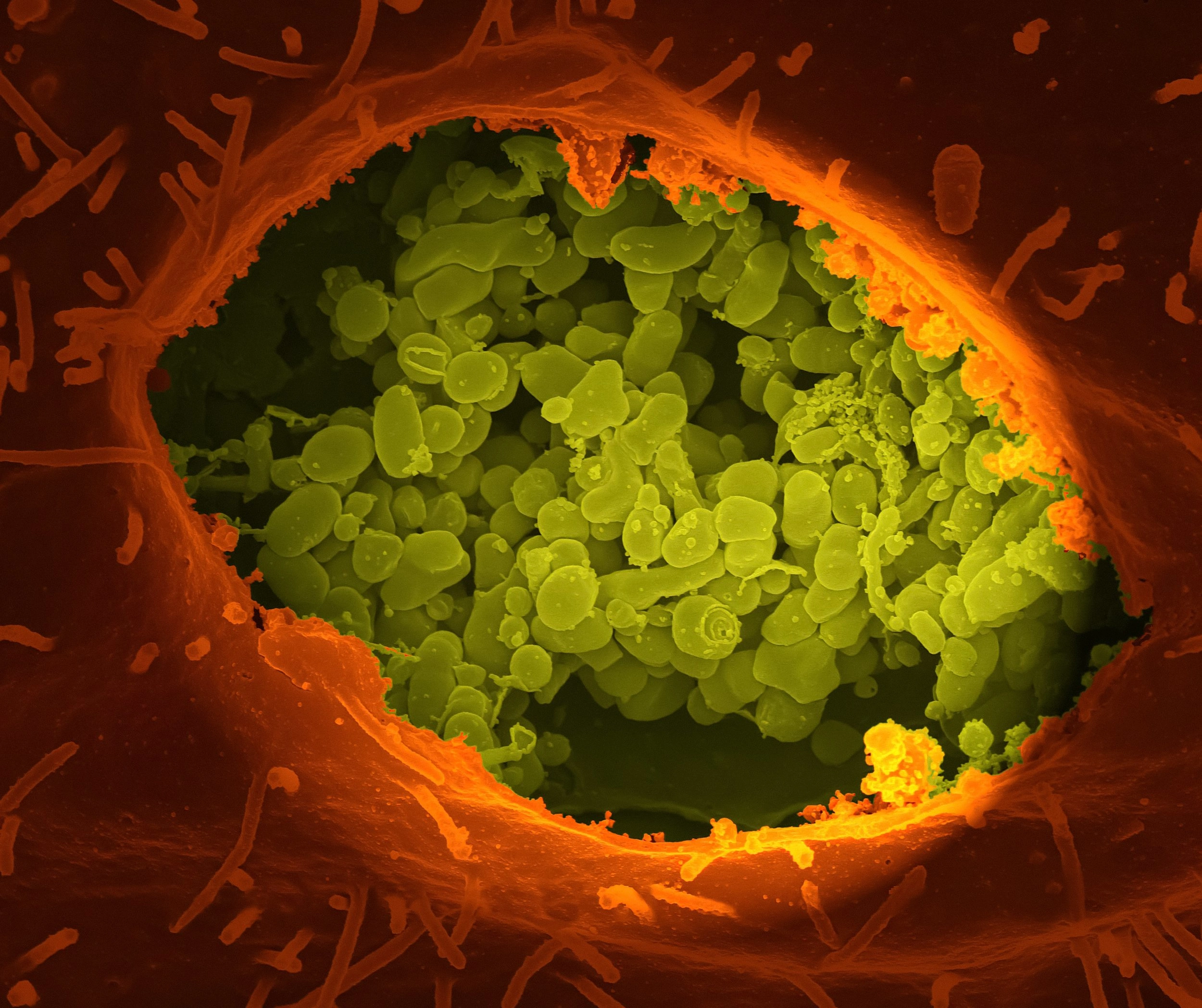
Bacteria usually are the culprit for infective endocarditis, but fungi, such as Candida, can also be the source of infection. Intravenous drug use is another source of endocarditis due to unsafe syringe use. Unsterile syringes contain bacteria that can enter the bloodstream, travel to the heart, and cause infection.
Current trends in IV drug use and endocarditis incidence
With drug deaths at an all-time high, endocarditis cases in drug users increased almost tenfold in the last decade. In 2011, there were approximately four cases of endocarditis per one million people suffering from opioid use disorder. In 2022, the rate of endocarditis in that group of individuals increased to 30 cases per day. And although rheumatic disease used to be the primary underlying disease for endocarditis, intravenous drug use is now one of the leading causes.
Endocarditis signs and symptoms
Many potential symptoms can result when an individual is first infected with endocarditis. The following flu-like symptoms typically develop first in the infected individual:
Fever
Sweats
Chills
Fatigue
There may be other symptoms, such as shortness of breath, cough, muscle/joint pain, loss of appetite, and weight loss.
Which diseases and defects increase the risk for endocarditis?
In high-risk individuals, bacteria that cause endocarditis can easily pass through the immune system and cause severe infection. The following diseases and scenarios can pose a higher risk for endocarditis:
IV drug users
Individuals with congenital heart disease
Those with a previous diagnosis of endocarditis
More common in men than in women
When to seek medical help
Seeking medical help at the start of any symptoms is critical to ensuring the infection does not conquer the patient’s immune system and heart—especially in high-risk individuals. If infected, hospitalization is required if symptoms are worsening.
Treating endocarditis
Treating endocarditis is simple but required to prevent the risk of fatality and other complications. Once admitted into the hospital, the patient receives antibiotics administered via an IV drip. The antibiotics can take two to eight weeks to eliminate the infection. If the individual is high-risk or the condition has progressed, treating it may take longer. In addition, sometimes abscesses can develop in the heart valves that need to be drained.
Complications of endocarditis
Proper treatment for endocarditis is crucial to reduce the risk of a variety of complications:
Stroke
Heart failure
Heart valve damage and a blood clot in the lung artery
Death
Also, bacteria can multiply, and heart valves can be damaged or destroyed without prompt antibiotic treatment. Heart valve repair or replacement is sometimes necessary for many patients previously infected with endocarditis.
Mitigating the risk for withdrawal in IV drug users with endocarditis
To reduce the risk of withdrawal in IV drug users, hospitals must increase protocols for treating endocarditis patients who use opioids illicitly. Withdrawal can happen when patients are admitted to the hospital without drugs, so a swift action plan and strong execution by medical personnel are vital.
A complex and unique approach to care with different specialists should be a priority, especially since addiction treatment is often separated from mainstream medical care. Addiction-trained clinicians must collaborate with cardiologists and other doctors to implement preventive measures, as subsequent endocarditis infection is likely in IV drug users. Appropriately mitigating the addiction and infection factors can prevent the individual from reinfection or extreme withdrawal.
Conclusion
The medical field has evolved exponentially over the past few centuries with significant improvements in medical devices and antimicrobial agents. Doctors and nurses—specifically cardiologists—are also better educated on how to treat endocarditis. Treatment effectiveness has also increased simultaneously with a greater understanding of pathobiology and epidemiology. Lastly, antibiotics are widely available and effectively treat endocarditis to prevent complications as severe as death.
There is significant hope for treating infections like this one. You are not alone—seek medical help even if you are unsure you need it. You never know when it might be too late.
About the Author
Matt Olszewski is a freelance writer in the Health and Medical fields based in Boston, MA. He graduated with a BA in Psychology and has work experience in clinical research. Bilingual in English and Spanish, he is currently studying at Tufts University for his MPH with a biostatistics and epidemiology concentration. During his free time, he loves going on runs, hikes, and exploring new cities.
Curious to learn more about the medical field and specifically cardiovascular health? Subscribe to my newsletter on my website!
Like this project
Posted Jul 26, 2023
Endocarditis infects and inflames the heart’s inner lining and compromises heart valves, often requiring repair or replacement. In the past, rheumatic fever …
Likes
0
Views
18
Tags





