Monkeypox virus: dangerous strain gains ability to spread throu…

Robel Getu
Copywriter
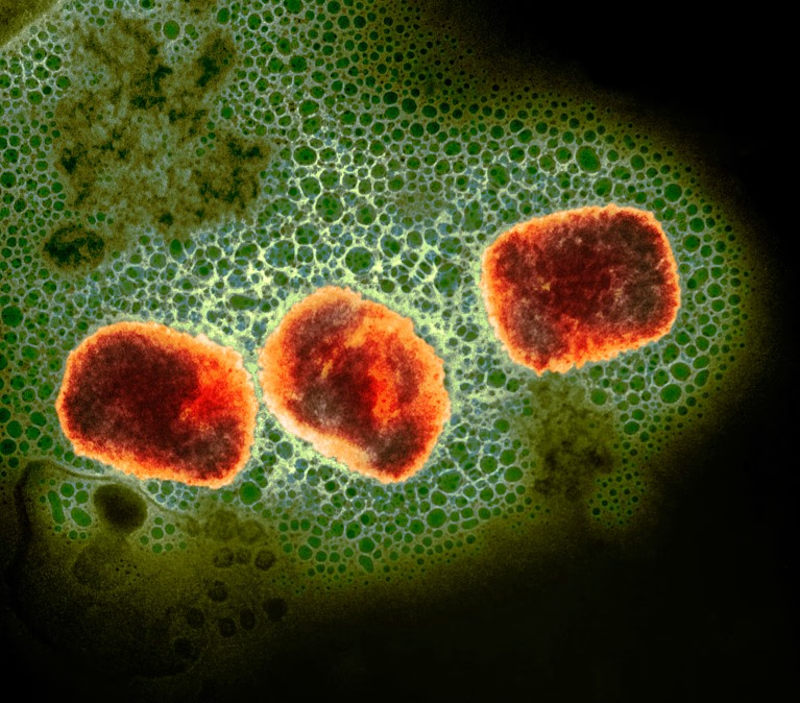
Monkeypox virus particles (artificially coloured).Credit: UK Health Security Agency/Science Photo Library
A virulent strain of the monkeypox virus has gained the ability to spread through sexual contact, new data suggest. This has alarmed researchers, who fear a reprise of the worldwide mpox outbreak in 2022.
Evidence from past outbreaks indicates that this strain, called clade I, is more lethal than the one that sparked the 2022 global outbreak. Clade I has for decades caused small outbreaks, often limited to a few households or communities, in Central Africa. Sexually-acquired clade I infections had not been reported before 2023.
But since then, a clade I strain with an apparent capacity for sexual transmission has caused a cluster of infections in a conflict-ridden region of the Democratic Republic of the Congo (DRC), in Central Africa. A preprint1 posted on 15 April reports that 241 suspected and 108 confirmed infections are connected to this outbreak — and these numbers are probably a vast undercount because of limited testing capacity. Almost 30% of the confirmed infections were in sex workers.
Adding to the challenges, the region is facing a humanitarian crisis, and the DRC is contending with the aggressive spread of other diseases, such as cholera. The combination means there is a “substantial risk of outbreak escalation beyond the current area”, says Anne Rimoin, an epidemiologist at the University of California, Los Angeles, who has worked on mpox outbreaks in the DRC since 2002.
Unheeded warnings
Monkeypox virus can cause painful, fluid-filled lesions on the skin and, in severe cases, death. (While the disease was renamed ‘mpox’ in 2022, the virus continues to be called ‘monkeypox virus.’) The virus persists in wild animals in several African countries, including the DRC, and occasionally spills into people.
The first large reported outbreak with human-to-human transmission, which was in 2017 in Nigeria, caused more than 200 confirmed and 500 suspected cases of the disease. Researchers warned at the time that the virus might have adapted to spread through sexual contact.
Their warnings were not heeded; in 2022, a global outbreak driven in part by sexual contact prompted the World Health Organization (WHO) to declare it a public health emergency. That ongoing outbreak is caused by a strain of monkeypox virus called clade II, which is less lethal than clade I, and has infected more than 94,000 people and killed more than 180.

Although mpox infections have waned globally since 2022, they have been trending upwards in the DRC: in 2023 alone, the country reported more than 14,600 suspected infections and more than 650 deaths. In September, 2023, a new cluster of suspected cases arose in the DRC’s South Kivu province. This cluster especially concerns researchers, as it has been spreading largely among sex workers, suggesting that the virus has adapted to transmit readily through sexual contact.
This could lead to faster human-to-human spread, potentially with few symptoms, says Nicaise Ndembi, a virologist at the Africa Centres for Disease Control and Prevention who is based in Addis Ababa. “The DRC is surrounded by nine other countries — we’re playing with fire here,” he says.
Health officials are so concerned that representatives of the DRC and 11 nearby countries met earlier this month to plan a response and to commit to stepping up surveillance for the virus. Only about 10% of the DRC’s suspected mpox cases in 2023 were tested, due to limited testing capacity, meaning health officials “don’t have a full picture of what’s going on”, Ndembi says.
Genetic analyses of the virus responsible for the outbreak show mutations such as the absence of a large chunk of the virus’s genome, which researchers have previously noted as a sign of monkeypox viral adaptation. This has led the study’s authors to give a new name to the strain circulating in the province: clade Ib.
Making matters more fraught, South Kivu borders Rwanda and Burundi and is grappling with “conflict, displacement, food insecurity, and challenges in providing adequate humanitarian assistance”, which “might represent fertile ground for further spread of mpox”, the WHO warned last year.
Vaccines and treatment needed
In 2022, many wealthy countries offered vaccines against smallpox, which also protect against mpox, to individuals at high risk of contracting the disease. But few vaccine doses have reached African countries, where the disease’s toll has historically been highest.
While the DRC weighs regulatory approval for these vaccines, the United States has committed to providing the DRC with enough doses to inoculate 25,000 people, and Japan has said it will also provide vaccines, says Rosamund Lewis, technical lead for mpox at the WHO in Geneva, Switzerland. But a vaccination drive in the DRC would require hundreds of thousands — if not millions — of doses to inoculate individuals at high risk of infection, she says.
It’s not clear how much protection these vaccines will provide against clade I mpox, but Andrea McCollum, a poxvirus epidemiologist at the US Centers for Disease Control and Prevention in Atlanta, Georgia, says that data from tests in animals are promising. Researchers are also conducting a trial in the DRC of tecovirimat, an antiviral that is thought to be effective against mpox. Results are expected in the next year, McCollum says.
The WHO and CDC have helped to procure equipment that will allow for more rapid diagnosis of the disease in the DRC, especially in rural areas, Lewis says. She adds that says the rapid mobilization of African health officials gives her hope that the outbreak can be controlled before clade Ib mpox starts spreading elsewhere.

